- Current updates relating to treatment for interstitial cystitis/bladder pain syndrome: systematic review and network meta-analysis - (https://pmc.ncbi.nlm.nih.gov/articles/PMC11040764/)
- Intravesical hyaluronic acid and chondroitin sulfate for recurrent urinary tract infections: systematic review and meta-analysis - (https://pmc.ncbi.nlm.nih.gov/articles/PMC6004275/)
- Changes In Urine Markers And Symptoms After Bladder Distention For Interstitial Cystitis - (https://pmc.ncbi.nlm.nih.gov/articles/PMC2373609/)
- Disease Course in Patients With Pentosan Polysulfate Sodium-Associated Maculopathy After Drug Cessation - (https://pmc.ncbi.nlm.nih.gov/articles/PMC7349079/)
About
Interstitial cystitis/painful bladder syndrome are terms used to describe urinary tract pain that is not caused by urinary infection or bladder stones. Since there are no exclusive symptoms for this condition, clinical diagnosis can be quite challenging.
Other Names (or Nomenclatures)- As the cause of Interstitial Cystitis (IC) is not fully understood, it has many names, and these include Bladder Pain Syndrome, Hypersensitive Bladder Syndrome, Painful Bladder Syndrome (PBS), Frequency-Urgency-Dysuria Syndrome, Chronic Pelvic Pain, and Urologic Chronic Pelvic Pain Syndrome (UCPPS).
Interstitial cystitis (IC) is a chronic condition that affects the urinary bladder.
IC/PBS is far more common in women than in men. According to a recent estimate,
1 million of the 1.3 million IC/PBS sufferers in America are women. In India, the man to woman ratio is 1:2.
Its symptoms, which include pelvic pain, pressure, and an urgent, frequent need to urinate, are often misunderstood as other, more common conditions like bladder infection or cystitis, or a stone in the urinary tract. The symptoms range from mild discomfort to severe, debilitating pain, which makes it even harder to figure out what's wrong.
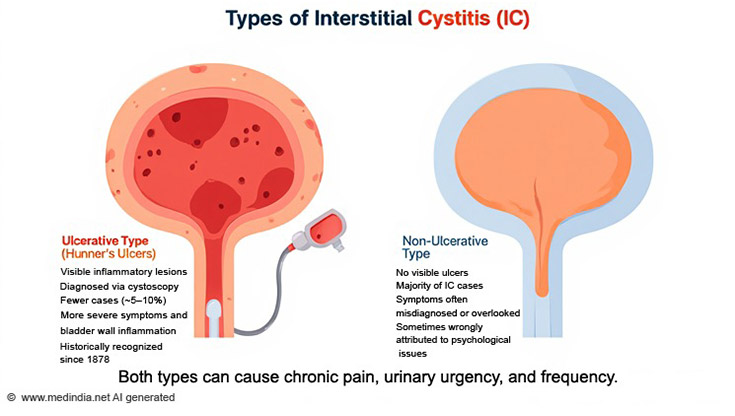
Two types of IC have emerged over the years -
- Ulcerative type of IC
- Non-Ulcerative type of IC
It wasn’t until 1978 that the non-ulcer variant gained medical acceptance, broadening the clinical understanding of IC/PBS. It is this type of IC that is very elusive when it comes to diagnosis.
Ulcerative type of IC
Hunner's ulcers, which are visible inflammatory lesions on the bladder wall, are a sign of a historically important type of IC, even though the symptoms are not always present. It can be identified through cystoscopy, and it defines the classic or ulcerative subtype of IC. Only a few percent of cases fall under this category, and the disease is usually diagnosed in individuals above 18 years, although there is no scientific basis for why IC cannot be present in children.
Hunner’s ulcers are not just superficial lesions; they are associated with more intense symptoms and a distinct inflammatory response.
The term interstitial cystitis was first introduced in a monograph by Skene in 1878. At first, the urologist looked for "elusive ulcers" on the bladder wall when they distended it for inspection using a cystoscope.
Non-Ulcerative type of IC
However, a majority of IC/PBS patients do not present with Hunner’s ulcer but instead come under the non-ulcerative subtype of IC, which is often misdiagnosed or dismissed and sometimes even attributed to psychiatric conditions.
The Role of Mast Cells and Epithelial Breakdown
In a healthy bladder, the outer layer (called the urothelium) acts like a watertight barrier. But in people with IC, this layer becomes leaky and allows irritating substances (like potassium) to pass through into deeper layers of the bladder.
This leakage triggers inflammation and activates certain immune cells called mast cells. These mast cells release chemicals like histamine and substance P, which cause pain and swelling.
As a result, the bladder nerves become extra sensitive, especially to stretching when the bladder fills. Over time, more pain-sensing nerve fibers (called C-fibers) grow, which adds to the chronic pain and sensitivity seen in IC.
Evolving Care for IC/PBS
Recent progress in understanding interstitial cystitis/painful bladder syndrome (IC/PBS), along with improvements in diagnosis and treatment, brings hope for better management and outcomes for patients.
Importantly, research provides some reassurance: there is no evidence that IC/PBS increases the risk of developing bladder cancer. It also does not affect fertility, nor does it impact the growth of the fetus during pregnancy.
Today, in the hope of providing more individualized treatment approaches in the future, research is being conducted to identify more specific subtypes, such as those determined by the presence or absence of ulceration, like Hunner's lesions.
Symptoms of IC/PBS
The elusive symptoms IC/PBS mimic many urinary conditions, including those of genitourinary system tuberculosis (TB), and previous therapies were focused on treating this condition. However, TB treatment does not provide any relief to the patients.
Hence, symptoms of IC are listed in some detail below:
Pain in IC
- Recurrent pain or discomfort, including throbbing, burning, or pressure sensation
- Pain may occur when the bladder fills with urine or gets emptied of it.
- Men also have pain when they ejaculate or when they experience an orgasm.
- Women may feel the pain during menstruation or vaginal intercourse.
The site of pain may be anywhere in the lower abdomen, pelvic region, in the urinary passage (urethra), back passage, or rectum. Hence, these different names are referred to this condition: Frequency-Urgency-Dysuria Syndrome, Chronic Pelvic Pain, and Urologic Chronic Pelvic Pain Syndrome (UCPPS).
Frequency & Urgency
Usually, in IC, frequency and urgency exist together, although urgency can exist on its own without frequency.
Frequency of urination is considerably increased in people with IC/PBS, mainly because their bladder cannot contain much urine, even if its size is normal.
If a person passes urine more than about 8 times in 24 hours, it is considered abnormal. Getting up at night to pass urine (nocturia) disturbs the sleep of the affected person. In extreme conditions, some patients may pass urine every 10 to 15 minutes and may describe their overall frequency as 40 to 60 times a day.
Incomplete emptying of urine or voiding is the other symptom that accompanies frequency and urgency
Symptoms of IC may get triggered or worsen in the following situations:
- Women often find that their symptoms get worse just before or during menstruation
- The symptoms may also worsen during menopause.
Food Triggering IC Symptoms
A certain type of food or drink may precipitate an attack or worsen the symptoms. These include:
- Coffee or caffeine
- Citrus fruits, Tomatoes
- Vinegar
- Alcohol
- Carbonated drinks
- Hot spices such as hot pepper and pickles,
- Foods with artificial sweeteners.
- Raw bulb onions
- Soybeans
Causes
The exact causes of IC/PBS are not properly understood. Scientists believe that it is a local (bladder) manifestation of a more general inflammatory condition involving other body organs, too.
It may be interesting to note that women with IC/PBS also suffer from illnesses, such as Fibromyalgia or Irritable bowel syndrome.
a) Chronic inflammation of the bladder wall
The Interstitial Cystitis Foundation (ICF), which was founded in 1995, describes the causes of IC as follows: Interstitial cystitis is generally caused by a chronic inflammation of the bladder wall and produces symptoms that wax and wane.
ICF estimates that an average person with IC consults SEVEN doctors before the condition gets correctly diagnosed.
Scientists aren't certain what triggers the inflammatory process; suspects include previous infections, unidentified substances in the urine, defects in the cells lining the bladder, disorders of nerve functions, activation of mast cells that can play an important role in allergic reactions, or a combination of these factors.
Whatever the cause, the affected bladder wall is hypersensitive to stimulation, and the presence of even a small amount of urine causes it to contract. As a result, discomfort is almost constant during flares of interstitial cystitis; pain and pressure are relieved only temporarily after responding to each urge to urinate.
b) Medical Conditions Associated with IC
There is a long list of medical conditions that may be associated with IC, and these include:
- Allergy
- Irritable bowel syndrome
- Sensitive Skin
- Vulvodynia
- Fibromyalgia
- Chronic Fatigue Syndrome
- Migraine
- Asthma
- Crohn's Disease/Ulcerative Colitis
- Systemic Lupus Erythematosus
- Rheumatoid Arthritis
Sjögren's Syndrome
Bacterial infection has been ruled out, although some of the IC/PBS symptoms closely resemble those of bacterial infection. Another reason for ruling out bacterial infection is due to the fact that the patients fail to respond to antibiotics.
Research is being carried out in this field to understand the causes, including the role of heredity, and to come up with better possible treatments for this elusive condition.
Diagnosis
As the symptoms of interstitial cystitis (IC)/painful bladder syndrome closely resemble other medical conditions, they should be ruled out, such as bladder cancer and urinary tract infection.
In women, endometriosis, which involves pelvic pain, must also be ruled out, while in men, chronic prostatitis (chronic pelvic pain syndrome) is the disease to look for before focusing on IC/PBS.
Frequency and urgency of urination, pain in the pelvic area, and absence of other treatable diseases are the pointers that could indicate IC/PBS.
For the first time in 2003, the severity of the different grades of disease was defined in Copenhagen.
The severity of IC depended on ‘cystoscopic visualization of the bladder mucosa.’ Severity was defined from no disease or normal to severe disease if it was grade IV.
- Grade 0 = normal mucosa
- Grade I = petechiae in at least two quadrants
- Grade II = large submucosal bleeding (ecchymosis)
- Grade III = diffuse global mucosal bleeding
- Grade IV = mucosal disruption, with or without bleeding/edema
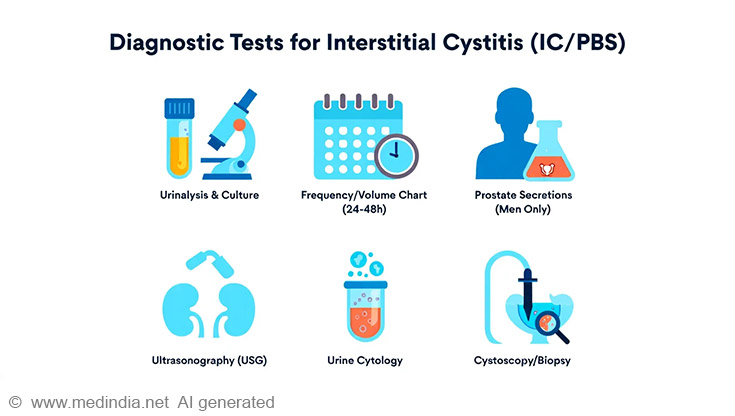
Diagnostic tests for IC/PBS
a) Urinalysis and Urine Culture
Examining urine under a microscope and culturing urine samples can help rule out urinary tract infections. If the symptoms continue to persist, despite the urine sample being sterile, IC/PBS might be suspected.
b) Frequency Volume Chart
A frequency/volume chart for 24 to 48 hours is a useful chart for assessment of the frequency and provides an objective evaluation of the symptoms.
c) Prostate Secretions
Prostatic fluid might be obtained from men (with no urinary infections) and allowed to be cultured to detect microbes causing prostate infection, which can be easily treated with antibiotics.
This is an uncommon test and is not frequently done. For this test, prostatic massage is required through rectal examination.
d) Ultrasonography (USG)
USG of the kidneys, ureter, and bladder with post-void residue may be carried out to rule out stones or urinary obstruction.
e) Urine Cytology
In this test, a sample of the patient's urine is centrifuged, and the sediments are seen under the microscope. It is a useful test to rule out malignancy of the bladder.
f) Cystoscopy/biopsy
This is an optional procedure in the diagnosis of interstitial cystitis (IC) and is usually performed as a final step to confirm the diagnosis.
During cystoscopy, a cystoscope-a specialized instrument-is used to directly visualize the bladder and check for any abnormalities. The cystoscope can be either rigid or flexible. Although both types can be used with local anesthesia in an outpatient setting, the flexible cystoscope is generally preferred because it causes less discomfort.
During the procedure, the bladder is distended (stretched) using sterile water or saline solution to improve visualization of its inner lining, which may cause significant discomfort or pain. For this reason, cystoscopy is typically performed under spinal or general anesthesia rather than local anesthesia to ensure patient comfort.
If present, Hunner's ulcers may be visible, though increased vascular markings are also common. After the bladder is stretched and begins to empty, mild, diffuse bleeding often occurs.
Many patients experience temporary relief for a few days or weeks following bladder distension. Additionally, to rule out bladder cancer, a biopsy (tissue sample) may be taken during cystoscopy and examined under a microscope.
Biopsy in Grade II to IV-if done, it may reveal a certain pattern of changes that indicates it to be a case of IC. These changes include:
- Presence of Mast cell count in the lamina propria layer of the bladder
- Complete loss of urothelial lining
- Granulation tissue in the lamina propria
- Increase in vascular density in lamina propria on factor VIII (F8) stain.
Treatment
Scientists have not yet found a definitive cure for IC/PBS.
Symptoms may vary with changes in diet and treatment. Sometimes they do so without a reason. They can appear, reappear, or disappear suddenly, and there is no way the doctors can predict the course of the disease or the way it responds to treatment.
Therefore, for now, all treatments are focused on relieving symptoms. Many patients benefit from a combination of treatments that are mentioned below(1✔ ✔Trusted Source
Current updates relating to treatment for interstitial cystitis/bladder pain syndrome: systematic review and network meta-analysis
Go to source)
a) Bladder Distention
As described earlier, the maximum distension of the urinary bladder has been found to bring relief to certain patients. Hence, some doctors would use this technique of bladder distention as the first therapy. It is thought that bladder distention interferes with the pain signals being transmitted by the bladder nerves.
In one study, they found that bladder distention altered urine anti-proliferative factor activity and heparin-binding epidermal growth factor-like growth factor (HB-EGF) levels towards normal, but the mechanism of symptom relief after distention is still unknown(3✔ ✔Trusted Source
Changes In Urine Markers And Symptoms After Bladder Distention For Interstitial Cystitis
Go to source).
However, if on cystoscopy (under anesthesia) the bladder capacity is less than 150 ml, a surgical augmentation of the bladder may be required.
b) Bladder Instillation
Bladder instillation, or intravesical therapies, is a popular way to provide relief to these suffering patients.
The medications are directly administered into the bladder via a urinary catheter. In this process, a solution is instilled in the bladder and left to be retained for some time, ranging from 10 to 15 minutes, after which it is emptied. The various substances include
Dimethyl Sulfoxide (Rimso-50), also called DMSO, is the only drug approved by the FDA for such a treatment. A urinary catheter is used to place the drug into the bladder, where it is retained for about 15 minutes and then expelled.
DMSO reduces inflammation, prevents muscle contractions, and reduces pain. The patient can be trained by a nurse or a doctor to do the procedure at home to make it convenient. There are minimal side effects of the drug. Urinary infection can occur if sterile technique is not used and may require antibiotics.
Side effects of DMSO include a garlic-like taste/odor on the breath and skin.
Other drugs are not approved by the FDA.
In India and other countries where RIMSO or DMDO is not available, some urologists have made their cocktail and have had some good results (unpublished and personal communication).
The agents include an anesthetic agent with a steroid, along with heparin and sodium bicarbonate to facilitate absorption. Like RIMSO, the solution is left in the bladder for 15-20 minutes, and a total of 6-8 treatments are given at intervals of 2 weeks.
c) Intravesical (Bladder Instillation) Therapies
- Intravesical Botulinum toxin injections (BOTOX):
The toxin causes some degree of neuromodulation. Usually, 200 to 300 units of botulinum toxin are injected in the bladder using a cystoscope at 20 to 30 locations (10 units per injection site). The injection may need to be repeated after 6 months. - Hyaluronic Acid (HA)
Restores the bladder's protective GAG layer. As reconstruction of the glycosaminoglycan layer plays a role in the successful treatment of bladder pain syndrome/interstitial cystitis (BPS/IC). - Chondroitin Sulfate (CS):
Often combined with HA, which is significantly more effective and better tolerated than long-term antibiotic use for preventing recurrent bacterial cystitis. It strengthens the bladder's protective GAG layer, reducing bacterial adherence and recurrence risk(2✔ ✔Trusted Source
Intravesical hyaluronic acid and chondroitin sulfate for recurrent urinary tract infections: systematic review and meta-analysis
Go to source). - Heparin
GAG-like compound used in bladder cocktails to protect the bladder lining. - Lidocaine
Local anesthetic is used for pain relief in instillation mixtures - Cocktail Therapies
In a treatise on the condition by Dr. Mishra, he has described using 40 ml of local anesthesia medication called Sensorcaine 0.5%, 20 ml of sodium bicarbonate, 2 cc of dexamethasone, and 10,000 units of heparin.
d) Neuromodulation & Nerve Stimulation
- Transcutaneous Electrical Nerve Stimulation (TENS): Nerves associated with the bladder can be mildly stimulated through electrical pulses. This can be either done through the skin (transcutaneous electrical nerve stimulation-TENS) or with the help of an implanted device.
It is not clear how TENS works, but it has been proposed that the electrical impulses might cause - Increase blood flow to the bladder
- Strengthen pelvic muscles controlling the bladder
- Trigger the release of pain-blocking substances
- Sacral Neuromodulation: A person can also have a device implanted that is capable of delivering impulses to the urinary bladder at regular intervals. The FDA has approved the device, which is being marketed as the Inter-Stim system. It helps to treat symptoms such as
- Urge incontinence,
- Urgency-frequency syndrome
- Urinary retention
- Percutaneous Tibial Nerve Stimulation (PTNS): A needle is placed near the ankle to stimulate the tibial nerve, affecting pelvic floor nerves.
e) Medications
Drugs that can be used to treat IC include:
- Pentosan Polysulphate Sodium (known as Elmiron)-100 mg 3 times a day-is the only FDA-approved oral drug specifically for IC.
- Antihistamines: Block histamine release, reducing bladder wall irritation.
- Antidepressants (amitriptyline): Reduce bladder pain and urgency by modulating nerve activity.
- Urinary analgesics
- Pain relievers/narcotics: Help control inflammation and pain.
- Gabapentin: Target nerve pain and reduce hypersensitivity.
It helps repair the bladder lining (GAG layer). It can be used for long-term treatment. However, it can rarely cause a vision-threatening maculopathy, a condition affecting the macula, the central part of the retina. This can lead to symptoms like blurred vision, difficulty reading, and problems with dark adaptation. PPS-associated maculopathy continues to evolve after drug cessation for at least 10 years. The prevalence can be 15%, as per a study(4✔ ✔Trusted Source
Disease Course in Patients With Pentosan Polysulfate Sodium-Associated Maculopathy After Drug Cessation
Go to source)
It may be prudent to consider drug holidays with Pentosan Polysulfate Sodium (PPS) to mitigate the risk of maculopathy.
Most drugs have side effects, and they must never be taken without consulting a doctor.
f) Diet
There is no scientific evidence associating dietary components with IC/PBS.
But it has been generally observed that certain foods aggravate the condition. They include-
- Alcohol,
- Chocolates
- Caffeine
- Citrus beverages/high-acid foods
- Tomatoes,
- Spices,
- Artificial sweeteners
g) Stress Management
Handling stress is crucial because it significantly exacerbates interstitial cystitis pain, urination urges, and frequent urination.
Meditation, mindfulness, and yoga can help ease stress and keep certain hormones at a level that’s less likely to cause strong bladder sensitivity.
People with chronic pain and associated emotional issues can benefit from cognitive behavioral therapy (CBT), while biofeedback helps them control their pelvic floor tightness and excessive cravings. By using these strategies, medical professionals can assist IC patients in reducing their symptoms and improving their quality of life.
h) Fluid Management
Controlled fluid intake, especially avoiding concentrated urine.
- Water is the best choice.
- Herbal teas like chamomile or marshmallow root are usually IC-safe.
- Avoid caffeinated, alcoholic, carbonated, and acidic drinks (e.g., coffee, cola, and orange juice), as they may trigger symptoms.
Sometimes, determining the food item that worsens the syndrome is important to dealing with the condition.
i) Smoking
Many sufferers of IC/PBS feel that smoking worsens the condition. It must also be remembered that smoking contributes to bladder cancer.
j) Exercise & Bladder Training
Gentle stretching exercises are known to bring relief to patients suffering from IC/PBS symptoms. Once the pain is controlled, the bladder can be trained to empty at regular intervals, or what is called timed voiding, with the help of relaxation techniques and distractions.
k) Support Groups
Interstitial cystitis does not have a cure, and for that reason, the individuals suffering from this condition are stressed a lot. The emotional support of family, friends, and fellow sufferers plays a large role in helping patients to cope.
It is also very important for the patient (and his family) to learn about the disease, to understand its dynamics, and to be involved in their treatment, as it will help them to tackle their problem in a better manner. When treating the challenging condition known as interstitial cystitis, it is appropriate to try a combination of several treatments clinically rather than just one. To determine the effectiveness of combined therapeutic approaches, such as immunomodulatory compounds, BTX or HA administered intravenously or by instillation, or HA and CS and dietary modification, more research is needed.
Below is a list of patient support groups for people with interstitial cystitis, painful bladder syndrome, and chronic pelvic pain.
The list of support groups maintained by the Interstitial Cystitis Association can be viewed at www.ichelp.org
https://www.ichelp.org/living-with-ic/support-community/us-support-groups/
https://rarediseases.org/organizations/interstitial-cystitis-association/
| COUNTRY | GROUP | MEETING SCHEDULE & LOCATION | CONTACT |
| Africa, Kenya | East Africa IC Support Group Nakuru Chapter | WHEN: Last Saturday of every month from 3:00 PM to 5:00 PM. Call to confirm meeting times and dates. WHERE: Mereca Hotel Nakuru Kenyatta Avenue. Also offer phone support for interested parties from patients to nurses, doctors, pharmaceutical companies and others. | James G. Mwangi jgmwangi2003@ yahoo.com 245720391104 |
| Argentina | ARACI Asociación Rosarina Afectados Cistitis Intersticial | Contact for support group meeting details. | Liliana Bacchi President menadel_dan@ hotmail.com 0341-4644164 Dorrego 3857-DTO.1 2000 Rosario, Argentina |
| Australia | IC Friends of Australia | A new Australian interstitial cystitis community forum has now been created to discuss life with IC and other related topics. The web address is - http://icfriends.forumotioncom | icfriends@live. com |
| Australia | Interstitial Cystitis Support Group of Australia | Contact Katya Buc. Please include your name and address. You may subscribe to receive the newsletter, which is published 3 times year at a cost of AU$7.00 per year. | Katya Buc PO Box 144, Richmond, VIC 3121 Australia |
| Austria | ICA Österreich e.V | www.ica-austria.at | [email protected] Christa Rammerstorfer, Chairwoman ica.at-rammerstorfer@ gmx.at Phone / Fax : 0043-7246-8448 |
| Bolivia | La Paz IC Support Group | Contact Maria. | Maria Eulalia Anker eulalia@ ceibo. entelnet.bo 5912-2712761 |
| Belgium | Interstitiële Cystitis Patiëntenvereniging België (ICPB) | www.icpb.be | Josée DE RAA, president [email protected] |
| Canada, Alberta | Available for phone support. | Ms. Edna Gabrielle 780-572-2233 | |
| Czech Republic | www.uroklinika.cz | Libor Zamecnik, MD, PhD [email protected] Urologicka klinika VFN a 1. LF UK Ke Karlovu 6 128 08 Praha 2 Czech Republic | |
| Denmark | Steinunn Joergensen Project Nurse Department of Urology [email protected] Herlev Hospital, University of Copenhagen DK-2730 Herlev, Denmark | ||
| England | Patient Advocate | Provides phone and email support, IC information, and healthcare provider referrals. | Iliana C. Brockman [email protected] |
| France, Paris | Association française de la cystite interstitelle | For information, please email http://orphanet.infobiogen.fr/ associations/AFCI See also "AFCI - Présentation" | Françoise Watel ci_france@hotmail. com AFCI 82 rue Albert 75013 Paris France |
| Mexico | Asociacion de Cistitis Intersticial Mexico | www.aci-mexico.com | Florentina Ferreyra Lopez flore@aci- mexico.com 52(55)54-04-89-16 Cerezos 87 casa 41 Col. Jardines de Atizapan Atizapan de Zaragoza, Edo. De Mex. Mexico CP 5297 |
| Netherlands | IC-Today | http://www.ic-today.com/ | Contact: Moenier Oulad, [email protected] |
Future Research
Research is being done to understand how the chemicals in the urine injure the bladder and the role of unidentified organisms in causing the disease.
Establishing a diagnosis of IC still seems to be a challenge, and many new markers are being established. Markers like antiproliferative factor (APF) and HP-EGF. EGF and insulin-like growth factor 1 are some of the markers that are being studied. Of all the markers, antiproliferative factor (APF) is the most studied. However, they have yet to have a clinical application.
To determine the effectiveness of combined therapeutic approaches, such as immunomodulatory compounds, BTX or HA administered intravenously or instillation, or HA and CS and dietary modification, more research is needed.
For more information on the clinical trials being carried out on IC/PBS, go to the following site:
www.ClinicalTrials.gov
 MEDINDIA
MEDINDIA

 Email
Email






