- Antoni Torres, Willy E Peetermans, Giovanni Viegi, and Francesco Blasi. Risk factors for community-acquired pneumonia in adults in Europe: a literature review. Thorax. 2013 Nov; 68(11): 1057–1065.
- Ivan Kuhajda, Konstantinos Zarogoulidis, Katerina Tsirgogianni, Drosos Tsavlis, Ioannis Kioumis, Christoforos Kosmidis, Kosmas Tsakiridis, Andrew Mpakas, Paul Zarogoulidis, Athanasios Zissimopoulos, Dimitris Baloukas, and Danijela Kuhajda. Lung abscess-etiology, diagnostic and treatment options. Ann Transl Med. 2015 Aug; 3(13): 183.
- Stop the Spread of Superbugs - (https://newsinhealth.nih.gov/issue/feb2014/feature1)
- Ruuskanen O1, Lahti E, Jennings LC, Murdoch DR. Viral pneumonia. Lancet. 2011 Apr 9;377(9773):1264-75 - (doi: 10.1016/S0140-67361061459-6. Epub 2011 Mar 22.)
- GC Mbata, CJ Chukwuka,1 CC Onyedum,1 BJC Onwubere,1 and EN Aguwa. The Role of Complications of Community Acquired Pneumonia on the Outcome of the Illness: A Prospective Observational Study in a Tertiary Institution in Eastern Nigeria. Ann Med Health Sci Res. 2013 Jul-Sep; 3(3): 365–369. - (doi: 10.1016/S0140-67361061459-6. Epub 2011 Mar 22.)
- Alexander Kallen, M.D., M.P.H., medical officer, U.S. Centers for Disease Control and Prevention; Mary Hayden, M.D., associate professor, pathology, Rush University Medical Center, Chicago, Ill.; Oct. 5, 2015, Journal of the American Medical Association - (doi: 10.1016/S0140-67361061459-6. Epub 2011 Mar 22.)
- Pneumonia - (https://www.nhlbi.nih.gov/health/health-topics/topics/pnu)
- Information About Pneumonia - (http://www.lung.org/lung-health-and-diseases/lung-disease-lookup/pneumonia/?)
- What is Pneumonia - (https://en.wikipedia.org/wiki/Pneumonia)
- Lobar pneumonia - (https://en.wikipedia.org/wiki/Lobar_pneumonia)
- Atypical pneumonia - (https://medlineplus.gov/ency/article/000079.htm)
- Overview Pneumonia - (http://familydoctor.org/familydoctor/en/diseases-conditions/pneumonia.printerview.all.html)
- Pneumonia: Guide to Your Recovery - (http://www.cpmc.org/learning/documents/pneumonia-ws.html)
- Top 20 Pneumonia Facts-2015 - (https://www.thoracic.org/patients/patient-resources/resources/top-pneumonia-facts.pdf)
What is Pneumonia?
Peripneumonia, and pleuritic affections, re to be thus observed: If the fever be acute, and if there be pains on either side, or in both, and if expiration be attended with pain, if cough be present, and the sputa expectorated be of a blond or livid color, or likewise thin, frothy, and florid…. When pneumonia is at its height…it is bad if he had dyspnea…and if sweat comes out about the neck and head, for such sweats are bad, as proceeding from the suffocation, rales, and the violence of the disease. - Hippocrates, [460-375 BC]
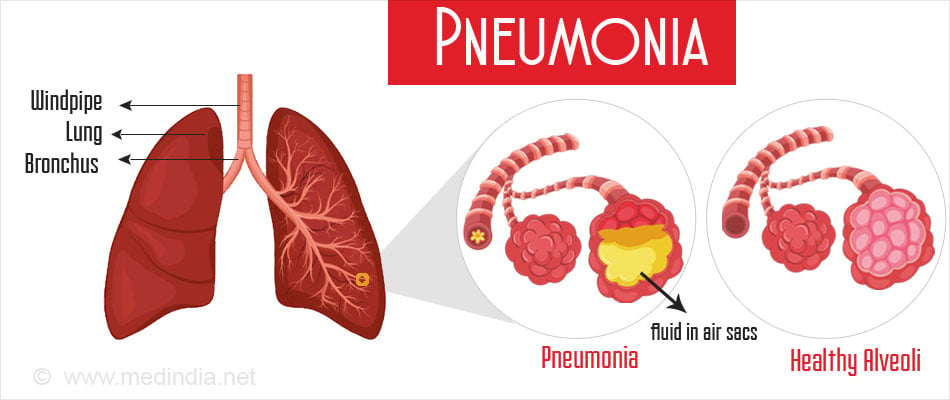
Pneumonia is infection of one or both lungs. It can be caused by bacteria, viruses, fungi and rarely by parasites. It is characterized by inflammation of the alveoli (air sacs of the lungs) that can be filled with fluid and/or pus.
It mostly occurs as a complication of a respiratory infection - like the flu. It is an infectious disease and can spread by coughing, sneezing or even breathing.
Pneumonia is one of the commonest causes of hospitalization and death in young children and elderly population.
Key Facts of Pneumonia
- Clinical Pneumonia is still the leading cause of childhood mortality in children accounting for 15% of all deaths of children under 5 years old. The number of children who died in 2015 was 920 136.
- Pneumonia can be caused by virus, bacteria, fungi or parasites.
- Community-acquired pneumonia (CAP) accounts for most hospitalizations and deaths worldwide
- Pneumonia can be prevented by vaccines building natural defences and curbing indoor air pollution
- Although, bacterial pneumonia can be treated with antibiotics, only one third of infected children receive the treatment.
- Anatomically pneumonia can be classified according to which part of the lung it affects.
- Bronchial pneumonia affects all parts of lung, while Lobar Pneumonia affects a large and continuous area of one lobe (caused mostly by Streptococcus pneumoniae).
- Noninfectious pneumonia or Idiopathic Interstitial pneumonia (IIP) affects the pulmonary interstitium (the tissue and space around the air sacs of the lungs). Some can affect the airways too. There are seven recognized subtypes for Idiopathic Interstitial pneumonia.
What are the Causes of Pneumonia?
Bacteria:
- Streptococcus (pneumococcus) (most common)
- Atypical bacteria - Legionella pneumophila, Mycoplasma pneumoniae, and Chlamydophila pneumoniae
- Other bacteria - Staphylococcus aureus, Moraxella catarrhalis, Streptococcus pyogenes, Neisseriameningitidis, Klebsiella pneumoniae, and Haemophilus influenzae
Virus:
- Influenza virus
- Coronavirus
- Adenovirus
- Rhinovirus,
- Respiratory syncytial virus (RSV)
- Parainfluenza virus
Bacteria like Streptococcus pneumoniae, Staphylococcus aureus, or Haemophilus influenzae can cause a secondary infection over the first viral one. All atypical symptoms of bacterial pneumonia get added on and there be serious complications.
Fungi:
- Histoplasma capsulatum
- Coccidiomycosis
- Blastomyces
- Aspergillosis
- Cryptococcus neoformans
- Pneumocystis jiroveci
Pneumonia caused by fungi is uncommon and occurs in persons with a weakened immune system. For example, Pneumocystis jiroveci usually causes pneumonia in people with impaired immune systems like HIV patients.
Parasites:
Do not cause pneumonia by specifically affecting the lungs. For example parasites belonging to Ascaris and Strongyloides genera stimulate a strong eosinophilic reaction, which may result in eosinophilic pneumonia.
One exception is Paragonimus westermani

How do you get Pneumonia?
Pneumonia is caused by breathing in small particles or droplets of the germs when exposed to a cough or sneeze of an infected person.
Sometimes during sleep secretions from the nose, throat or mouth (that contain viruses and bacteria) can be aspirated into the lungs and this can lead to pneumonia.
People with a weak immune system or inability to fight infections, can contract pneumonia easily that can become quite severe.
The most common way to get pneumonia is from crowded environments like schools, malls or a market place. This is called Community-acquired pneumonia (CAP) and is the leading cause of hospitalization and death due to pneumonia in the world.
Pneumonia can be contracted as a secondary infection by a patient who is already in the hospital being treated for another illness (Hospital - acquired pneumonia (HAP)).
Similarly places like nursing homes, dialysis centers and outpatient clinics are high-risk places to contract the disease (Healthcare-associated pneumonia). Being on a ventilator in a hospital can also cause pneumonia (Ventilator-associated pneumonia).
Persons who have brain injury, Alzheimers, swallowing problems or sometimes in a post-operative recovery time may end up inhaling their food as opposed to ingesting it. This is termed Aspiration Pneumonia and is another way to get the lung infection.

What are the Risk Factors of Pneumonia?
Risk factors for pneumonia include:
A child 2 years or younger or an adult 65 years and above
- Having a cold, laryngitis, influenza or other viral respiratory infections
- Having a weakened immune systems due to Human immunodeficiency virus (HIV), organ transplant, chemotherapy or long-term steroids treatment.
- Suffering from a chronic disease like asthma, emphysema, Chronic Obstructive pulmonary disease (COPD), cystic fibrosis, heart disease, diabetes, cerebrovascular disease, chronic liver or renal disease.
- Intensive care unit (ICU) patients and especially if they are on a ventilator
- Smoking
- Consumption of alcohol
- Exposure to dust, chemicals, air pollution or toxic fumes as they can compromise lung function making them more susceptible to infections
- A patient with swallowing problems
due to stroke, dementia, Parkinson#$#s disease, or other neurological conditions - History of recent surgery or trauma
- Suffering from epilepsy or seizures
What are the Symptoms of Pneumonia?
Symptoms of bacterial pneumonia in healthy people happen suddenly and progress rapidly starting during or after an upper respiratory infection.
In contrast, nonbacterial pneumonia symptoms happen gradually and are milder in nature.
- Persistent cough - in some cases of pneumonia the sputum can be thick and greenish yellow or it can be a bloody mucus
- Fever as high as 1040C
- Headache and muscle aches.
- Shaking chills
- Fatigue and loss of appetite
- Shortness of breath
- Chest pain on inspiration
- Confusion or delirium in older adults
In children the body can be slightly cyanosed (more bluish) due to poorly oxygenated blood and the child could be quite ill.

How can we Diagnose Pneumonia?
Physical examination - A coarse breathing sound like wheezing along with rales (crackling sounds or rumblings) may be heard on examining the patient’s chest with a stethoscope (Chest auscultation). Breathing can be labored or rapid too.
Further diagnosis of pneumonia can be done with the help of the following tests depending on the severity of the disease and the overall health and age of the patient -
Sputum examination to determine the causative organism. The sample or mucus is taken after a deep cough and seen under a microscope. It can also be cultured to know the type of organism and its sensitivity to antibiotics.
Complete Blood count (CBC) to check for an increase in the white blood cell count (positive if over 10,000 or >10×109 white cells per liter)
C-reactive protein level - positive if 3 times above the normal range. Indicates inflammation and is a non-specific test.
Chest X-Ray - to determine the location and extent of pneumonia in the lungs. Infection will be seen only when the disease has progressed. In some cases, it shows the organism causing pneumonia, complications of the disease and fluid accumulation in the chest cavity.
Bronchoscopy to look into the lung’s airways. In this procedure a thin flexible tube is Inserted into the nose or mouth while using a local anesthetic. Specimen of tissue and fluid can be collected for investigation.
An arterial blood gas (ABG) test to check for oxygen level in the blood from the lungs and a pulse oximetry to check how much oxygen is circulating via the bloodstream
Pleural fluid culture to check if there is fluid in the space around the lungs
CT scan to check the extent of pneumonia infection in a persistent or complicated case.
How can Pneumonia be Treated?
The treatment for Pneumonia depends on the causative organism, severity of the symptoms, age and overall health.
There is no specific cure for viral pneumonia since antibiotics do not work against viruses. It usually heals by itself in 1-3 weeks with rest and plenty of fluids.
Adequate intake of fluid helps to keep lung secretions thinner and easier to cough up. If the cough is non-productive and painful, cough suppressants can be used - or else it is better to cough it out as it is a protective mechanism to expel sputum.
- Fever can be controlled by acetaminophen, ibuprofen or aspirin.
- Viral pneumonia caused by the Influenza A or B viruses are treated by Neuroaminidase inhibitors. For other community acquired pneumonias like coronavirus, adenovirus and parainfluenza virus, there are no antiviral medications.
- Pregnant women who acquire pneumonia after a flu may get antiviral medications like oseltamivir (Tamiflu) or zanamivir (relenza) to relieve symptoms.
Discovery of antibiotics in the last 50 years has dramatically improved the treatment of bacterial pneumonia. The infection usually clears up in 2-3weeks.
Bacterial pneumonia can be treated at home by antibiotics.

Initially the doctor would prescribe a broad-spectrum antibiotic like penicillin or erythromycin group of derived antibiotics like ampicillin (Augmentin) can be used.
For example, in the UK, amoxicillin is usually the first line of treatment for Community-associated pneumonia (CAP) and doxycycline or clarithromycin are alternatives.
In the US, where “atypical” forms of CAP are more common, amoxicillin has been completely replaced by macrolides (azithromycin or erythromycin) and doxycycline in adults. Children still continue to be treated with amoxicillin. Patients responding well to the antibiotics get better within 2-3 days.
Hospitalization may be required if the patient has not recovered and the symptoms continue or become more severe. This happens specifically if the patient is older than 65 or younger than 2 or has a chronic illness.
β-lactam such as cephazolin plus macrolide (azithromycin) or a fluoroquinolones is used. The addition of corticosteroids also appears to improve outcomes. Both traditional 7-10 days of treament or a shorter course of 3-5 days work.
For hospital-acquired pneumonia, third- and fourth-generation cephalosporins, carbapenems, fluoroquinolones, aminoglycosides, and vancomycin are given intravenously and used in combination.
How do we Prevent Pneumonia?
Pneumonia can be a deadly disease depending on the type. Preventive measures and proper treatments can cut down child deaths due to pneumonia by around 1million worldwide.
Vaccines
Vaccines are an effective method to prevent the disease. Even if a person acquires pneumonia after the vaccine their symptoms will be milder with fewer complications.
Influenza Vaccine
The Influenza vaccine that helps prevent the flu is given annually in October or November, before peak flu season.
Since the flu is an underlying cause for pneumonia, the vaccine cuts the chance of people getting pneumonia.
Pneumococcal Pneumonia Vaccine
- A vaccine against Streptococcus pneumoniae prevents pneumonia in children and adults. It is recommended for:
- Adults 65 years old or older.
- Persons with chronic diseases, serious long-term health problems or weak immune systems.
- Smokers
- Children less than 5 years old.
- Children, 5–18 years of age with predisposed medical conditions like heart or lung diseases or cancer.
- Patients who have their spleen removed should be vaccinated to decrease the risk of postsplenectomy sepsis (OPSS) due to organisms like as Streptococcus pneumoniae, Haemophilus influenzae type B, and Neisseria meningitidis. They require to be vaccinated with a polyvalent vaccine to reduce the morbidity and mortality of postsplenectomy infection.
Hib Vaccine
The Hib vaccine protects people from getting infected by Haemophilus influenzae type b (Hib) that can cause pneumonia and meningitis.) The vaccine is given to children younger that 5 years old starting at 2 months of life.
Vaccines against pertussi, varicella and measles have a protective effect against pneumonia too.

Other factors that can prevent pneumonia:
- Hand hygiene – regular hand washes
- Covering nose and mouth while coughing and sneezing
- Reducing indoor air pollution
- Not smoking
- Breastfeeding children up till 6 months of age
- Strong immune system
- Physical activity
- Healthy diet
What are the Complications of Pneumonia?
Pneumococcal infections can be “invasive” or invade other disease free parts of the body. In such cases, complications can arise that may be deadly or result in long-term problems.
Meningitis - a serious complication of pneumonia that causes inflammation of the meninges (membrane covering the brain and spinal cord). About 1 in 15 children less than 5 years old acquiring pneumococcal meningitis either dies or acquires a long-term problem like hearing loss or developmental delay. The risk increases in elderly patients.
Symptoms include a stiff neck, fever, headache, pain when looking into bright lights and confusion.
Bacteremia - a complication that occurs when the bacteria infect the blood. Death occurs in about 1 out of 100 children younger than 5 years old. The risk increases in elderly patients. Symptoms are fever, chills and low alertness. This bacteria can then enter other organs causing organ failure.
Sepsis: When the bacteria affect the entire body.
Massive Pleural Effusion and Empyema- Pleural effusion is when there is excess fluid accumulation in the pleural space present in between the lungs and chest cavity. When microorganisms infect this fluid and pus is formed it is termed empyema.
Lung Abscess - when cavities form in the lung. These cavities contain necrotic debris and pus.
Bronchiolitis obliterans (BO) - when the smallest airways of the lungs or bronchioles get obstructed due to inflammation, this blocks free flow of air into the lungs.
Acute Respiratory Distress Syndrome (ARDS) - is not a disease but a medical condition that is characterized by widespread inflammation in the lungs.
A non-invasive pneumococcal infection is one that does not include bacteremia or empyema. Deaths occur in about 5 out of 100 people in this category. The risk increases with elderly patients.
Middle ear infections, Sinusitis and bronchitis - Non-invasive kinds of pneumococcal infections that are milder but more common.
Increasing pneumococcal resistance to antibiotics underlines the importance of vaccination.
What is the Future of Antibiotic Treatment of Pneumonia?
More and more bacteria are becoming resistant to antibiotics due to overuse of these medications by doctors and also due to self-medication in some unregulated countries.
These antibiotic resistant bacteria are called “superbugs”. These are the bugs or bacteria that survive the fight against the antibiotics either due to incomplete course of an antibiotic treatment or because doctors prescribe antibiotics for fevers that are not caused by bacteria.
Superbugs get passed on between individuals.
A new antibiotic resistant bacteria called CRE or Carbapenem-resistant Enterobacteriaceae resists some of the widely used antibiotics.
In the context of pneumonia, Klebsiella pneumoniae is an enterobacteriaceae that produces an enzyme that breaks down the antibiotic. This would delay treatment of pneumonia and the patient might develop severe complications.
To help curb the rise of antibiotic resistant bacteria, antibiotics should be prescribed when required and in this situation the full course should be taken.

















