- Overview prostate cancer - (http://www.mayoclinic.org/diseases-conditions/prostate-cancer/home/ovc-20317957)
- What is Prostate Cancer? - (https://www.cancer.org/cancer/prostate-cancer.html)
- Prostate cancer - (https://en.wikipedia.org/wiki/prostate_cancer)
- What you need to know about prostate cancer - (http://www.prostate.org.au/awareness/general-information/what-you-need-to-know-about-prostate-cancer/)
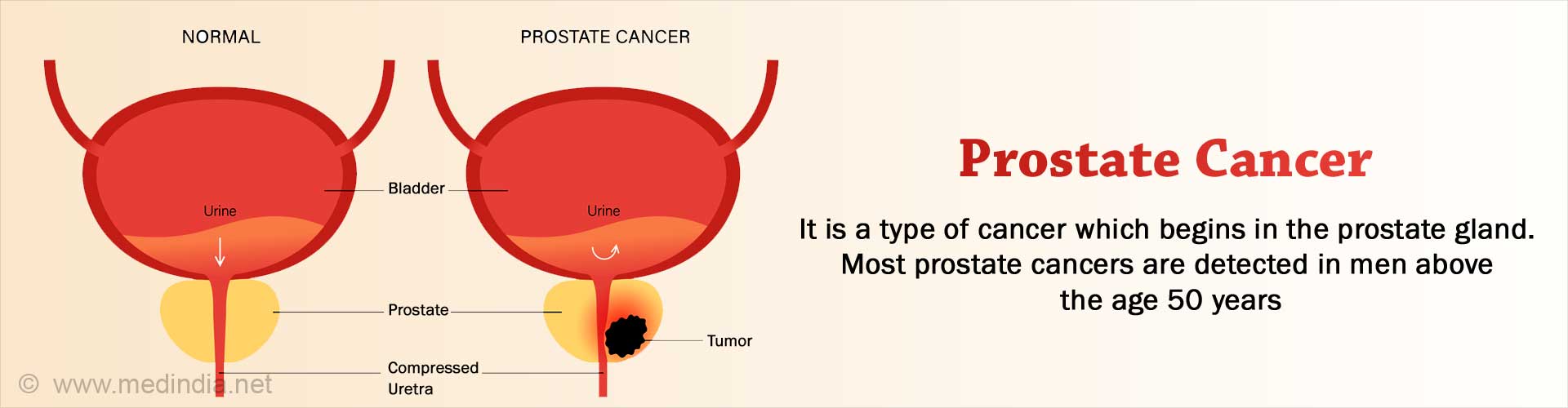
What is Prostate Cancer?
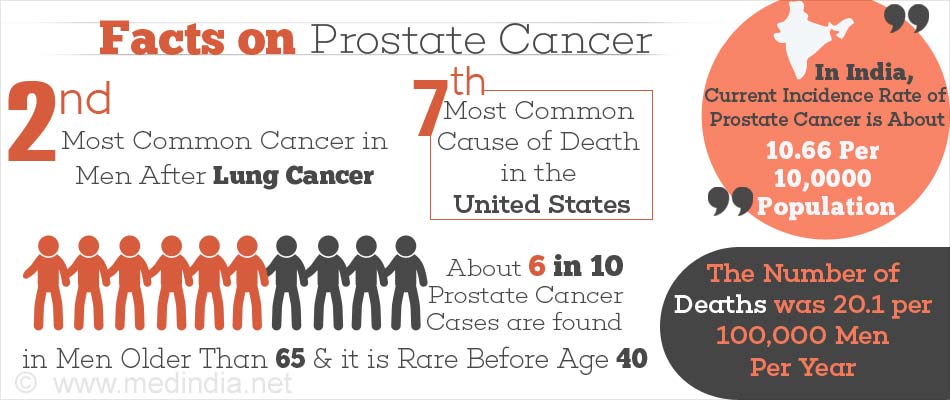
Prostate cancer is the second most common cancer in men after lung cancer. The natural history of the cancer is different from other cancers of the body. The most common prostate cancer is a slow growing cancer that does not necessarily kill the patient. The less common aggressive form especially in the younger age group has a more sinister growth pattern and needs to be picked up early to treat it effectively.
Prostate cancer usually does not give rise to any symptoms till it is in an advanced stage. Any man over 50 years who undergoes health screening should insist to have their prostate checked as generally it is not part of a routine health package. This requires a simple rectal examination and sometimes a blood test called PSA.
Incidence of Prostate Cancer
The incidence of the cancer in men goes up with their age and in men who are over the age of 80 years, it is almost 80%. Prostate cancer incidence has been going up due to improving longevity.
- It is estimated that approximately 1 in 7 men will be diagnosed with prostate cancer during their lifetime, however only 1 in 33 will die of this disease.
- Overall prostate cancer is the seventh most common cause of death in the United States.
- About 6 in 10 cases are diagnosed in men aged 65 or older,
- The average age at the time of diagnosis is about 66.
- The number of deaths was 20.1 per 100,000 men per year.
Until the last century prostate cancer was considered a rare disease – most likely due to shorter life expectancy and poordiagnostic methods. With the aging world population the burden of disease due to the prostate has gone up and is expected to show a further rise in the coming years.
“Blacks have twice the rates of prostate cancer death as Caucasian men,For reasons we don't know, it also starts at a younger age in African-American men." ~ Harmon Eyre
What are the Risk Factors for Prostate Cancer?
While the causes of prostate cancer are not yet completely understood, researchers have found several factors that are consistently associated with an increased risk of developing this disease.
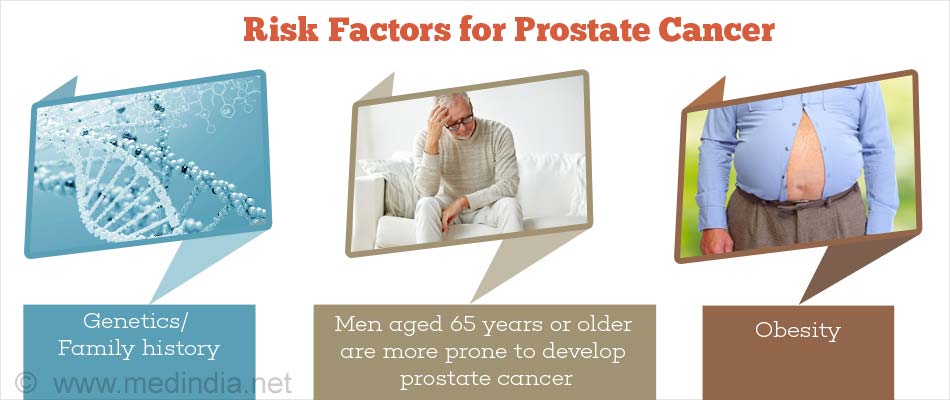
Prostate cancer seems to run in some families, suggesting an inherited or genetic factor.
Having a father or brother with prostate cancer usually doubles a man's risk of developing this disease. The risk is even higher for men with several affected relatives, particularly if they were young at the time of diagnosis.
Research and follow up studies has shown that although some factors increase a person's risk of getting prostate cancer but they do not always cause the disease. On the other hand, many people with one or more risk factors never develop the cancer but others with no risk factors develop the cancer
The chance of having prostate cancer increases after the age of 50. Hence screening is being considered for this age group although mass screening is expensive and may not be practical to be carried out in a large community.
What are the Causes of Prostate Cancer?
What causes prostate cancer is still not known exactly but, researchers have found some risk factors and are making progress toward understanding how these factors cause cells in the prostate gland to become cancerous.
During the past few years, scientists have made great progress in understanding how certain changes in DNA can cause normal prostate cells to grow abnormally and form cancers. DNA are chemical strands that carry the instructions for nearly everything our cells do. We usually resemble our parents because they are the source of our DNA. However, DNA affects more than our outward appearance. Some genes (parts of our DNA) contain instructions for controlling when cells grow and divide.
Certain genes that promote cell division are called oncogenes. Others that slow down cell division or cause cells to die at the appropriate time are called tumor suppressor genes. It is known that cancers can be caused by DNA mutations (defects) that turn on oncogenes or turn off tumor suppressor genes. Some people with certain types of cancer have DNA mutations they inherited from a parent. Researchers have recently found that inherited DNA changes in certain genes make them more likely to develop prostate cancer. These genetic changes appear to be responsible for about 10 per of prostate cancers.
DNA mutations related to prostate cancer usually develop during a man's life rather than having been inherited before birth.
What is the Role of Hormones in Prostate Cancer development?
There is evidence that development of prostate cancer is linked to increased levels of certain hormones. High levels of androgens (male hormones) may contribute to prostate cancer risk in some men. Researchers have recently noted that men with high levels of another hormone, insulin-like growth factor-1 (IGF1), are more likely to develop prostate cancer.
What are the Symptoms of Prostate Cancer?
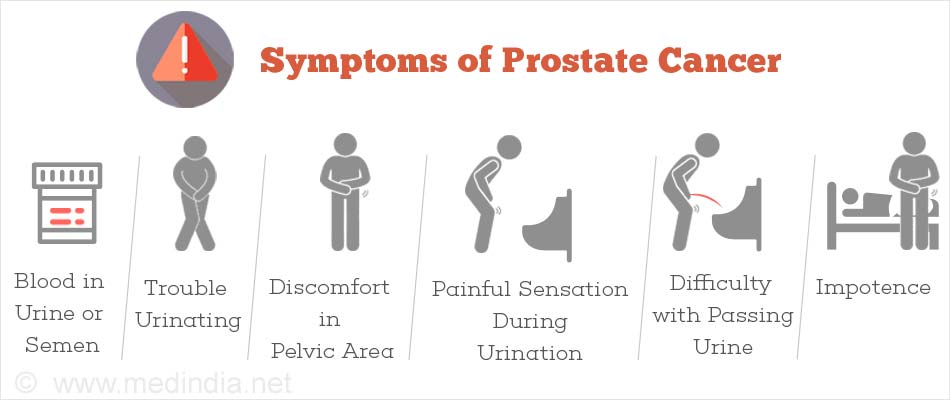
A small percentage of patients with prostate cancers may present with symptoms such as slowing or weakening of the urinary stream or the need to urinate more often. However in such cases often the cancer may have spread to other regions of the body.
- Trouble urinating
- Blood In The Urine,
- Impotence
- Pain In The Pelvis, Spine, Hips, or Ribs
These symptoms may also be present with other diseases.
How to Diagnose for Prostate Cancer?
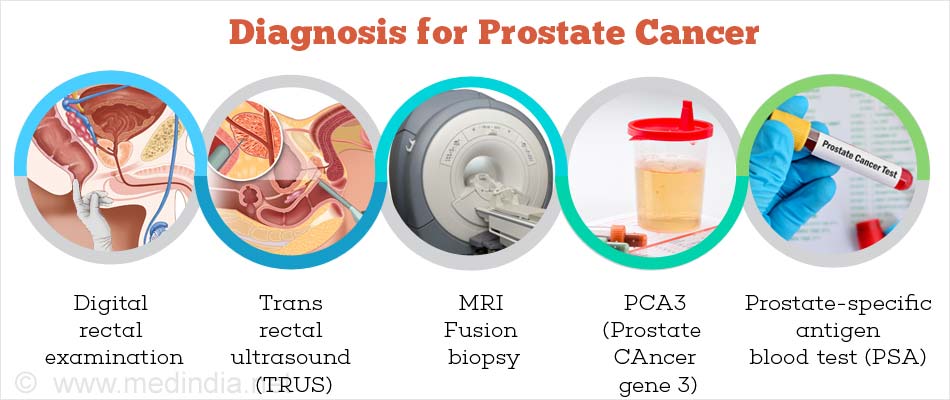
A digital rectal examination (DRE) can tell if the gland is cancerous or benign. A cancerous gland will feel hard and be unyielding
Prostate-specific Antigen Blood Test
This blood test to measure PSA - a protein which is made by prostate cells. It is recommended that men over the age of 50 years should have it checked annually. This is a must if there is a family history of the cancer.
PSA blood test results are reported as nanograms per milliliter (ng/ml). Results under 4 ng/ml are usually considered normal. Results over 10 ng/ml are high and values between 4 and 10 are considered borderline. The higher the PSA level, the more likely the presence of prostate cancer.
High levels of PSA usually indicates the likely chances of a man having prostate cancer but other conditions such as infection of the prostate gland or benign prostate hyperplasia (non-cancerous prostate enlargement) can also cause a rise in PSA. On the other hand in a highly aggressive prostate cancer the PSA maybe normal.
Several medications and herbal preparations can also lower blood PSA levels. Men with a high PSA result are advised to have a biopsy, to find out whether or not cancer is present.
After surgery or radiation treatment for prostate cancer, a rising PSA levels can provide an early sign that the cancer is coming back.
What is Digital Rectal Examination and How is it Done?
The prostate gland is located in front of the rectum and can be felt by inserting a finger in the rectum. Most cancers begin in the part of the gland that can be reached by a rectal exam. The exam causes no pain and only takes a minute to do.
The doctor inserts a gloved, lubricated finger into the patient's rectum and feels for any irregular or abnormally firm area that might be a cancer. This examination procedure is called a digital rectum examination (DRE).
If the DRE result is abnormal, a biopsy is recommended regardless of the PSA levels. The DRE is also used once a man is known to have prostate cancer, in order to help predict whether the cancer has spread beyond his prostate gland. It is also used to detect cancer that has come back after treatment.
Transrectal Ultrasound
Transrectal ultrasound (TRUS) uses sound waves to create an image of the prostate on a computer screen.
Sound waves are released from a small probe placed in the patient's rectum. The sound waves create echoes as they enter the prostate. The same rectal probe detects the echoes that bounce back from the prostate and a computer translates the pattern of echoes into a picture.
Because prostate tumors and normal prostate tissue often reflect sound waves differently, this test may be useful in detecting tumors, even those which might be too small or located in areas of the gland that cannot be felt by rectal examination. Occasionally the ultrasound may not be able to differentiate normal from cancerous tissue. The procedure is essentially painless and takes about 10-20 minutes. The procedure is essentially painless and takes about 10-20 minutes.
TRUS is useful when the PSA or DRE indicates an abnormality, to guide the biopsy needle into exactly the right area of the prostate.
The prostate biopsy
A biopsy is a surgical procedure that removes a sample of tissue for examination. A core needle biopsy is the main method used to diagnose prostate cancer. Under transrectal ultrasound guidance a doctor inserts a thin gauze needle through the wall of the rectum into the area of the prostate gland that appears abnormal. The needle then removes a cylinder of tissue, which is then tested under microscope. The procedure takes about half an hour and causes little discomfort.
When Prostate Cancer is Confirmed?
If cancer is found in a prostate biopsy, it is graded in order to estimate how fast it is likely to grow and spread. Prostate cancers are graded according to how closely they look like normal prostate tissue.
How Do You Stage of Prostate Cancer?
If cancer is found in a prostate biopsy, it is graded in order to estimate how fast it is likely to grow and spread. Prostate cancers are graded according to how closely they look like normal prostate tissue.
What is Gleason System of Grading?
The most commonly used prostate cancer grading system is called the Gleason system. This system assigns a Gleason grade ranging from 1 through 5 based on how much the arrangement of the cancer cells mimics the way normal prostate cells appear. If the cancer cell clusters resemble the small, regular, evenly spaced glands of normal prostate tissue, a grade of 1 is assigned. If the cancer lacks these features and its cells seem to spread haphazardly through the prostate, it is a grade 5 tumour.
Cancers with a high Gleason score are more likely to have already spread beyond the prostate gland at the time they are detected. Therefore, the Gleason score along with the blood PSA level and DRE is useful in considering treatment options.
The highest and lowest grade frequency in the gland is reported and 2 scores are provided. Thes are added together and the maximum score can be 10 - if the tumor is highly aggressive throughout the gland. Most tumors usually have a score of 7 or 8.
If the prostate biopsy finds a cancer, more tests are done to find out how far the cancer has spread. This is called staging of the cancer. The stage of a cancer is the most important factor in choosing treatment options.
Physical Examination
The physical exam, especially the digital rectal examination, is an important part of prostate cancer staging. The DRE feel can tell an experienced surgeon whether the cancer is limited to one side of the prostate or is present on both sides.
Imaging tests used for prostate cancer staging
Computed Tomography
Commonly known as a CT or CAT scan, this test uses an x-ray beam to create a series of pictures of your body from any angles. A computer combines the information from all these pictures to produce a detailed cross-sectional image. This may reveal abnormally enlarged lymph nodes. Lymph nodes are a network of bean-sized collections of white blood cells that fight infection. Some prostate cancers spread to nearby lymph nodes, called pelvic lymph nodes. Enlarged pelvic lymph nodes could be a sign of spreading cancer, or could mean that your body is fighting an infection.
Magnetic Resonance Imaging (MRI)
MRI uses magnetic fields to create detailed cross-sectional pictures of selected areas of your body. These pictures can show abnormal areas of bones or lymph nodes that suggest cancer may have spread from the prostate.
Radionuclide Bone Scan
This procedure helps show whether the cancer has spread from the prostate gland to bones. The patient receives an injection of radioactive material. This low level of radiation does not cause any side effects. The radioactive substance is attracted to diseased bone cells throughout the entire skeleton. Areas of diseased bone will be seen on the bone scan image as dense, gray areas, called "hot spots".
Lymph Node Biopsy
This procedure is done to find out if cancer has spread from the prostate to nearby lymph nodes. Lymph nodes may be removed by the surgeon through an incision in the lower part of the abdomen and test them for cancer or through laparoscopy. In most instances the lymph nodes are removed at the same time as the removal of the prostate to avoid unnecessary anaesthesia.
Very rarely a sample of cells from a lymph node is taken by using fine needle aspiration (FNA), in which CT scan images guide a long, thin needle into the lymph nodes. The syringe attached to the needle takes a small tissue sample from one of the lymph nodes. There is no incision, no scar, and the patient can return home a few hours after the proceed
The TNM Staging System
While there are several different staging systems for prostate cancer, the most commonly used system is the TNM system. It describes the extent of the primary tumor (T stage), the absence of spread to nearby lymph nodes (N stage), and the absence or presence of distant metastasis (M stage).
How Do You Treat Prostate Cancer?
Once prostate cancer has been diagnosed, graded, and staged, there is a lot to consider before you choose a treatment plan. The treatment you choose for prostate cancer should also take into account your age and expected life span, personal preferences and feelings about the side effects associated with each treatment, any other serious health conditions you have, and the stage and grade of your cancer.
Methods of Treatment
- Surgery
- Radical prostatectomy
- Retropublic Prostatectomy
- Radical Perineal Prostatectomy
- Tran urethral resection of the prostate
- Cryosurgery
- Radiation therapy
- Hormone therapy
- Chemotherapy
- Watchful Waiting
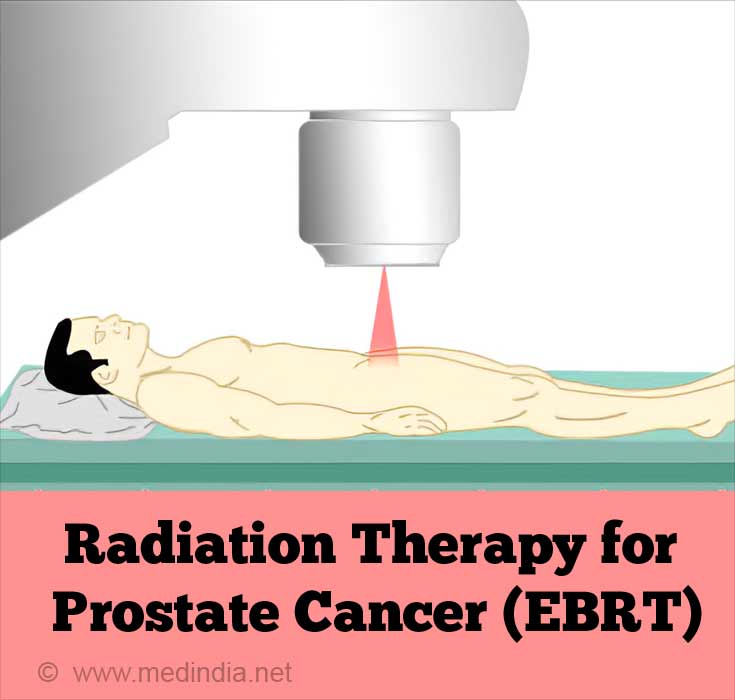
Radiation therapy
Radiation therapy uses high-energy rays (such as gamma rays or x-rays) and particles (such as electrons, protons, or neutrons) to kill cancer cells. Radiation is sometimes used to treat cancer that is still confined within the prostate gland, or has spread to nearby tissue. If the disease is more advanced, radiation may be used to reduce the size of the tumor and to provide relief from present and future symptoms.
Radiation usually eliminates the need for surgery and avoids the surgical side effects like impotency and urine leakage. Patients who do not have a good response to radiation therapy may still opt for surgery at a later date.
Radiation therapy can come in different forms.
There are essentially two main types of radiation therapy -
- External beam radiation (ERB)
- Brachytherapy (internal radiation)
The advanced forms tend to cause less damage to the surrounding tissues and produce better results in the long run. Three-dimensional conformal radiation therapy (3D-CRT) uses special software from computers to precisely locate the prostate gland and the radiation beams are then aimed at the prostate from several directions. This approach is likely to cause less likely to damage normal tissues.
Another form of External beam radiation is called Intensity modulated radiation therapy (IMRT).
In IMRT, a computer-driven machine moves around the patient as it delivers radiation in 3D form. IMRT is the most common type of EBRT for prostate cancer. The technique allows to deliver higher dose of radiation to the cancer compared to the normal tissue.
The cyber-knife and proton beam therapy are the latest form of external radiation therapy.
Hormone therapy
In the early 1940s two doctors, Huggins and Hodges, won the Nobel Prize for Medicine for their discovery that most prostate cancer cells are dependent on the male hormone testosterone for nourishment.
Combination hormone therapy (CHT) means the use of two drugs to control the bodies production of testosterone. It is the most widely used of several variations of hormone therapy. CHT combines the drugs to reduce or eliminate or block the effects of the production of testosterone from the testicles and adrenal glands.
Chemotherapy
This is used for patients whose prostate cancer has spread outside of the prostate gland and for whom hormone therapy has failed. These patients are in advanced statge of the disease.
Chemotherapy is not expected to destroy all the cancer cells, but it may slow tumor growth and reduce pain. It is not recommended as a treatment for men with early prostate cancer.
Chemotherapy uses anti-cancer drugs that are injected into a vein, injected into a muscle, or taken orally. These drugs kill cancer cells, but they also damage some normal cells.
Sometimes, hospitalization may be needed to monitor the treatment and to control its side effect.
Watchful Waiting
It is generally agreed that prostate cancer is a slow-growing cancer and sometimes may not require an aggressive approach. Most men with prostate cancer die of other causes before they ever experience symptoms of the disease.
Watchful waiting allows the patient and their doctor to watch for progress of the cancer and make decisions about more aggressive treatment if need for such treatments is indicated by a rise in PSA or appearance of symptoms. This type of treatment maybe advocated for patients with limited life expectancy or if the tumor is of low grade.
Surgery for Prostate Cancer
The two most common prostate operations are radical prostatectomy and transurethral resection of the prostate. Recent advances with minimally invasive approach means that the prostate can be removed using a laparoscopic method or using a robotic method.
Robotic radical prostatectomy is now one of the commonest surgeries performed for prostate cancer. The patients can usually be discharged the next day after the surgery. The complication rate is lower, however it is more expensive than open surgical procedure.
Radical Prostatectomy
This procedure removes the entire prostate gland plus some tissue around it. Radical prostatectomy is used most often if the cancer is thought not to have spread outside of the gland. The patient is generally put under general anesthesia or under spinal or epidural anesthesia during the surgery.
There are two main types of radical prostatectomy radical retro pubic prostatectomy and radical perineal prostatectomy. In the retro pubic operation, the surgeon makes a skin incision in the lower abdomen. The surgeon can remove lymph nodes during this operation through the same incision.
Radical Retro Public Prostatectomy
A nerve-sparing radical retro pubic prostatectomy is a modification of this operation. During this procedure, the surgeon carefully preserves the small bundles of nerves on either side of the prostate gland. If the cancer has not spread to these nerves, the surgeon will not remove them. Because these are the nerves that are needed for erections, leaving them intact lowers the risk of impotence following surgery.
Radical Perineal Prostatectomy
The radical perineal prostatectomy removes the prostate through an incision in the skin between the scrotum and anus.
These operations last from two to four hours. This is followed by an average hospital stay of three days and average time away from work of three to five weeks. In most cases, you will be able to donate your own blood before surgery. This blood can be given back to you during the operation, if needed.
All the patients will have a catheter is inserted through the penis and into the bladder after surgery while the patient is still asleep. The catheter stays in place for 10 to 21 days and allows good healing before it is removed. After the catheter is removed youou will be able to urinate on your own after the catheter is removed.
Tran Urethral Resection of the Prostate
Tran Urethral Resection of the Prostate can be used to relieve urinary symptoms caused by a cancer before other treatments begin. But it is not expected to cure this disease or remove all of the cancer.
This operation removes part of the prostate gland that surrounds the urethra. It is most often used to treat men with non-cancerous enlargement of the prostate called benign prostatic hyperplasia. An endoscopic tube with a small loop of cautery wire on the end is placed inside the prostate through the urethra. Electricity is passed through the wire to heat it and cut the tissue. Either spinal anesthesia or general anesthesia is used. The operation usually takes about one hour.
A catheter is inserted through the penis into the bladder after surgery. It remains in place for two or three days to help urine drain while the prostate heals. You can usually leave the hospital after one to two days and return to work in a week or two. There may be some bleeding into the urine after surgery anesthesia used.
Cryosurgery
Cryosurgery, also called cryotherapy or cryoablation, is used to treat localized prostate cancer by freezing its cells with a metal probe. Warm saline water is circulated through a catheter in the urethra to keep it from freezing. The probe is placed through a skin incision located between the anus and scrotum, and guided into the cancer using transrectal ultrasound. The appearance of prostate tissue in ultrasound images changes when it is frozen. Spinal or epidural anesthesia is used during the procedure.
The catheter is removed on to two weeks later. After the procedure, there will be some bruising and soreness of the area where the probe was inserted. Men usually remain in the hospital for one or two days.
What are the Side Effects of Surgical Treatment of Prostate Cancer?
Incontinence
Incontinence is the inability to control the urine stream, resulting in leakage or dribbling of urine. The patient may have urine leakage when coughing, laughing, sneezing, or exercising. Treatment of incontinence depends on its type, cause, and severity. Options include exercises to strengthen bladder muscles, biofeedback, medications, and additional surgery. Normal bladder control returns for many patients within several weeks or months after radical prostatectomy. Mild stress incontinence may persist permanently after surgery in up to 35 percent of men.
Impotence
Impotence, also known as erectile dysfunction, is an inability to get an erection of the penis. The nerves that allow men to get erections may be damaged or removed by radical prostatectomy. Radiation therapy and cryosurgery can also cause damage to these nerves. However, after the first 3 to 12 months after radical prostatectomy, most men will not be able to get a spontaneous erection if the nerves have been preserved.
Side Effects of Cryosurgery
Freezing can damage nerves near the prostate and cause impotence and incontinence. These complications occur about as often after cryosurgery as they do after radical prostatectomy. In addition, freezing may damage the bladder and intestines to some extent, leading to pain, a burning sensation, and the need to empty the bladder and bowels often. About 50 percent of men notice swelling of their penis and scrotum after cryosurgery, usually lasting a couple of weeks.
Side Effects of Radiation Therapy
Both during and after treatment side effects may include frequent urination, burning sensation while urinating and blood in the urine. Radiation therapy may also cause a feeling of fatigue that may not disappear until a month or two after treatment stops. Impotence usually does not occur right after radiation therapy but gradually develops over one or more years.
Diarrhoea with or without blood in the stool may also be present. Occasionally, normal bowel function does not return after treatment is stopped.
Side Effects of Chemotherapy
The side effects of chemotherapy depend on the type of drugs, the amount taken, and the length of treatment. Temporary side effects might include nausea and vomiting, loss of appetite, loss of hair, and mouth sores. Because chemotherapy can damage the blood-producing cells of the bone marrow, patients may have low blood cell counts. This can result in an increased change of infection. Most side effects, however, disappear once treatment is stopped.
Side Effects of Hormone Therapy
- Hot flashes similar to those experienced by women in menopause, It may sometimes controllable with other drugs such as Menace.
- Breast enlargement, which may be prevented by treatment with radiation to the breasts prior to the start of the hormone blockade treatments.
- Impotence-varying degrees are experienced. Generally, potency returns hormone therapy is discontinued. Actually, loss of libido is experienced more often than impotency.
- Other possible side effects include, anemia, weight gain, loss of muscle mass, loss of body hair, and diarrhea.
Diet and Prostate Cancer
Whether or not diet can help in the prevention or cure of prostate cancer is a very difficult question to answer. In terms of prevention, the answer may be yes, but there is very little hard scientific evidence to be sure. However, a lack of scientific evidence does not necessarily mean a lack of benefit, but simply that very little research has been performed in this area. There is a great deal anecdotal evidence which points to diet as benign a major factor in accelerating the disease.
Vegetarians are approximately half as likely to develop prostate cancer as meat eaters. It is not clear why this should be the case. It is not clear whether meat itself is the problem or whether a person who eats more meat is less likely to eat other beneficial foods for example.
It is observed that people in eastern countries such as India, China and Japan are far less likely than westerners to develop cancer. Also, the levels of cancer in the east are arising and this coincides with changes in lifestyle since more people are eating western style foods. Blacks who get prostate cancer have a more aggressive form and it is more common in them than it is in the white population.
What's New in the Research Field?
WA 'vaccine' that pits immune system against prostate cancer.
By injecting prostate cancer patients with a genetically engineered 'vaccine', researchers at the Johns Hopkins Oncology Center in Baltimore, Maryland, have activated the immune system against the disease.
Such a complete and through activation of the immune system against prostate cancer has never before been seen, according to study senior author Dr. William G. Nelson, of the Johns Hopkins University School of Medicine. The study was published in the October 15th issue of the journal Cancer Research.
The Johns Hopkins researchers focused on eight prostate cancer patients whose cancers had spread throughout the body despite surgical removal of the prostate.
Using cells taken from these patients, the researchers grew prostate cancer cells in the laboratory. They then injected a potent anti-cancer gene, GM-CSF, into these cells. Then they reintroduced the cancer cells back into the patient. The cells were irradiated prior to injection to eliminate the possibility of triggering new cancers.
Within a month after injection, the cancer 'vaccine' had placed each patient's immune T-cells on 'high alert' against prostate cancer cells.
The researchers "were not surprised to see T-cell activation," Nelson said in a Johns Hopkins statement, since T-cells are naturally 'turned on' by the presence of retroviruses such as the one carrying the vaccine.
Side effects were minimal: Mostly itching at the injection site and flu-like symptoms.
The researchers believe the therapy holds promise as a new method of attacking metastatic (spreading) cancers. "Using gene therapy, we re-educated the immune systems to recognize prostate cancer cells as a potential infection and attack," explained study lead author Dr. Jonathan Simons.
He believes that genetically-engineered vaccines "could make a real difference when used as secondary therapy".
 MEDINDIA
MEDINDIA
 Email
Email
























what are the chances of prostate cancer after the age of 69yrs.