- Foot Drop Information Page - (https://www.ninds.nih.gov/Disorders/All-Disorders/Foot-Drop-Information-Page)
- Foot Drop - (https://www.ncbi.nlm.nih.gov/books/NBK554393/)
- Treating Foot Drop in People With Multiple Sclerosis Using Electrical Stimulation - (https://clinicaltrials.gov/ct2/show/NCT02123537?term=Foot+Drop&draw=2&rank=1)
- Foot Drop Treatment (Tendon Transfer) - (https://www.footcaremd.org/conditions-treatments/midfoot/foot-drop-treatment-tendon-transfer)
- Medical Tests Foot drop - (https://www.ucsfhealth.org/medical-tests/foot-drop)
- Foot drop - Diagnosis & Treatment - (https://www.mayoclinic.org/diseases-conditions/foot-drop/diagnosis-treatment/drc-20372633)
- About Foot Drop - (https://my.clevelandclinic.org/health/diseases/17814-foot-drop)
- Foot Drop Recovery: Understanding All Of Your Options - (https://www.saebo.com/blog/foot-drop-recovery-understanding-options/)
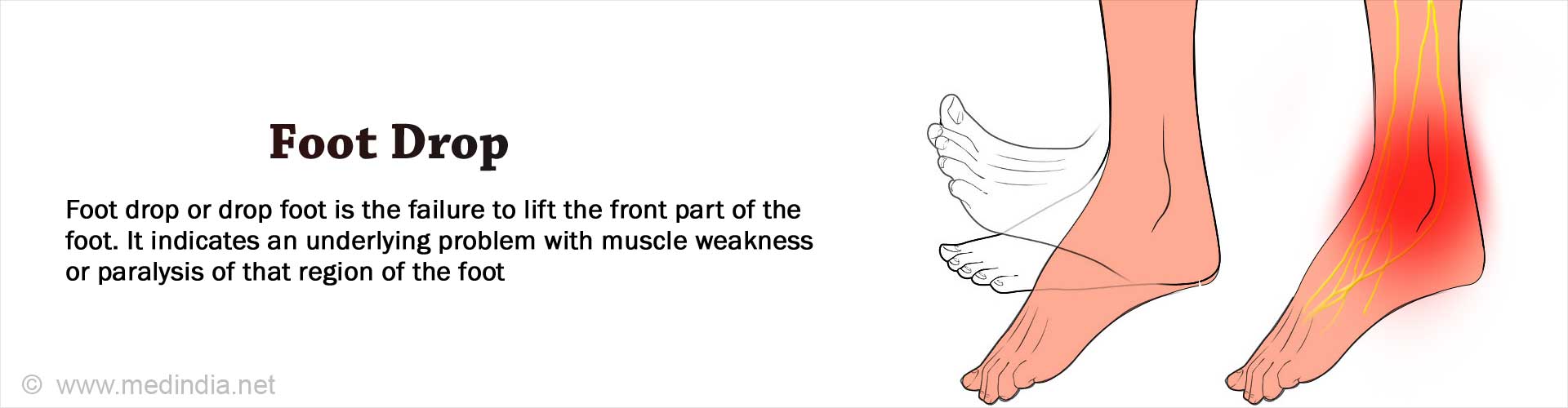
What is Foot Drop?
Foot drop, also referred to as drop foot, is the inability to lift the foot, especially the front part of your foot (forefoot). This typically results in dragging the foot on the ground during walking.
Foot drop is not a disease but a sign of underlying pathology, that produces weakness or paralysis of the muscles associated with raising the foot (dorsiflexion). It may strike one foot (unilateral) or both feet (bilateral). This may provoke unsteadiness in walking with frequent falls.
Grading of Foot Drop
The differing gradations of muscle weakness witnessed in foot drop may be classified as per MRC:
- 0 = complete paralysis,
- 1 = flicker of contraction,
- 2 = contraction with gravity eliminated alone,
- 3 = contraction against gravity alone,
- 4 = contraction against gravity and some resistance, and
- 5 = contraction against powerful resistance (normal power).
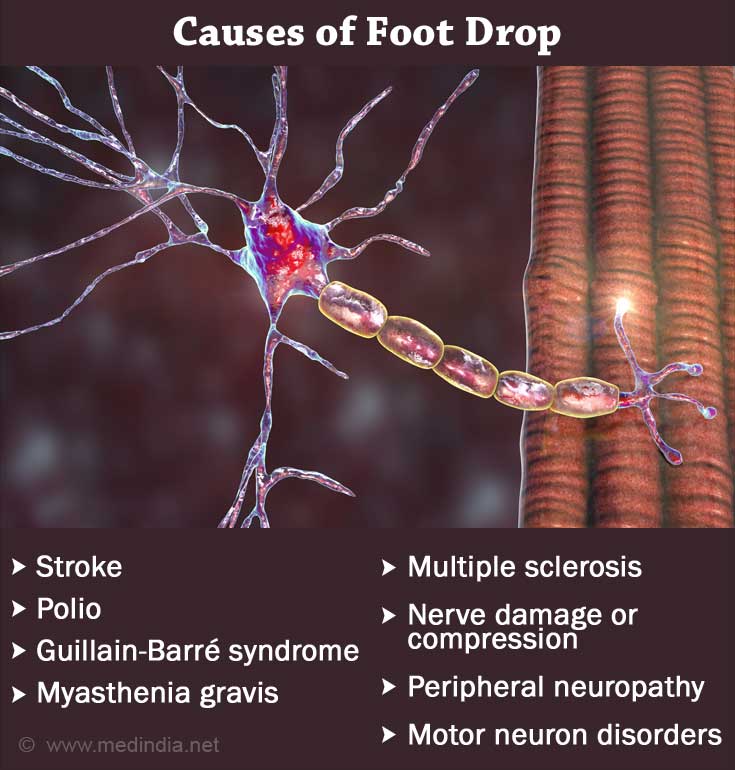
What are the Causes of Foot Drop?
Any weakness or paralysis of the muscles responsible for lifting the foot, results in foot drop. Depending upon the causal factors, foot drop can be either temporary or permanent. These include:
- Myasthenia Gravis (a neuromuscular disorder that attacks the junction between nerve and muscle)
- Motor neuron disorders such as
- Polio (poliovirus affects the spinal cord, resulting in paralysis)
- Spinal muscular atrophy (hereditary disease that destroys neurons vital for muscle activity)
- Amyotrophic lateral sclerosis (also known as Lou Gehrig’s disease affects nerve cells in the brain and spinal cord)
- Peripheral neuropathy (affects nerves of legs and hands)
- Damage to peripheral nerves like peroneal nerve (responsible for sensation and movement of legs)
- Compression of other nerves of the leg like fibular nerve and sciatic nerve
- Guillain-Barré syndrome (acute inflammatory demyelinating polyneuropathy – AIDP)
- Charcot-Marie-Tooth disease (type of neuropathy)
- Multiple sclerosis (an autoimmune disorder that affects the protective covering of nerves)
- Stroke (poor blood supply to the brain causes region-specific functional damage)
- Cerebral palsy (impairs the ability to move, balance, and maintain posture)
- Muscular dystrophy (results in loss of muscles and their strength)
- Myositis (inflammation of the muscles)
- Spinal stenosis (spinal cord narrowing causes injury to the nerve roots resulting in "pinched nerve")
- Lumbar radiculopathy (lumbar disc herniation or spondylitis causes damage to the spine and exiting nerves)
- Bony or tumor overgrowth in the spinal canal
- Somatization disorder (functional cause)
What are the Symptoms & Signs of Foot Drop?
- Difficulty in lifting the front part of your foot
- Dragging the foot when walking
- Hitting the foot to the ground on placing it through each step
- High steppage gait (lifting your legs or thigh unusually higher as if climbing stairs)
- Lack of sensation in the foot
- Numbness
- Loss of muscles/ muscle wasting in legs and feet
What are the Risk Factors of Foot Drop?
Factors that may cause compression/damage to the peroneal and other nerve supplying the leg result in foot drop. These are:
- Trauma or leg fractures
- Abdominal or pelvic surgery
- Hip or knee replacement surgery
- Diabetes
- Crossing your legs
- Prolonged squatting or kneeling
- Leg cast
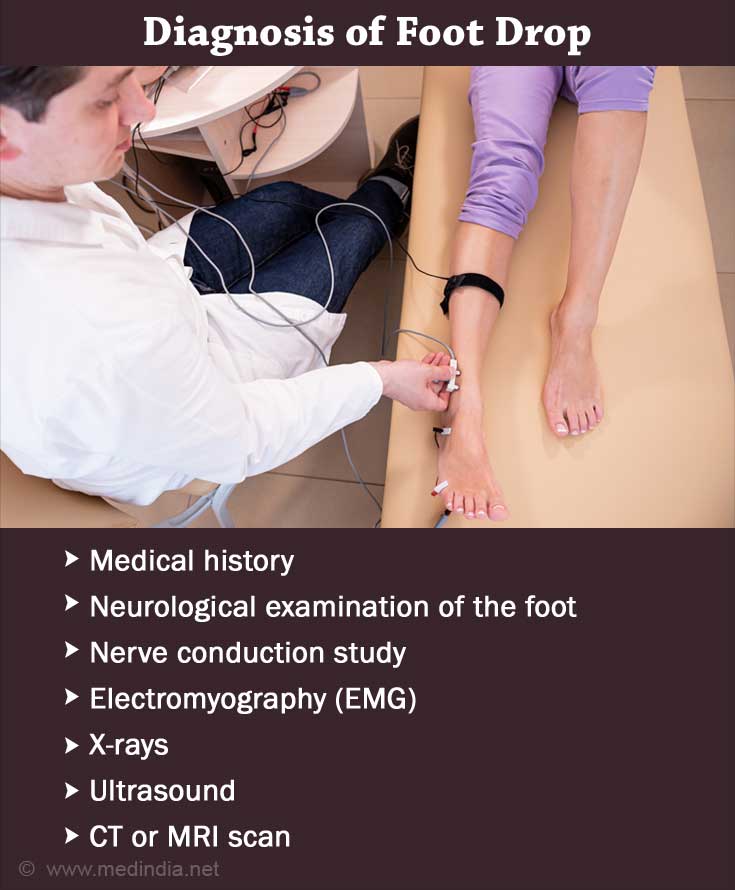
How do you Diagnose Foot Drop?
- Careful medical history
- Detailed neurological examination of the foot, muscles, and gait.
- Sensory tests to rule out any loss of sensation and numbness in the foot.
- Nerve conduction study: It is a test to estimate the velocity and conductance of electrical impulses through your nerves. In other words, examine the functioning of the nerves. A patch of an electrode is attached to the skin (area of interest) and a mild voltage is used to stimulate the nerve. This further aids in diagnosing the extent of nerve damage.
- Electromyography (EMG): A comparatively painful test that involves inserting a small needle (electrodes) into the muscle (through the skin). The affected nerve is further stimulated to measure the electrical activity in the muscles, and nerves. It is the gold standard test to rule out any neuromuscular basis for foot drop.
- Imaging tests like X-rays to rule out bony growth
- Ultrasound: Sound waves are used to investigate the presence of any cysts or tumors that may cause nerve compression.
- CT scan
- Magnetic resonance imaging (MRI): Serves in detailed visualization of the pathology of the soft tissues as a cause for nerve compression.
- Blood tests to rule out diabetes and the presence of any potential toxins that may cause foot drop.
- Psychiatric evaluation to rule out somatization
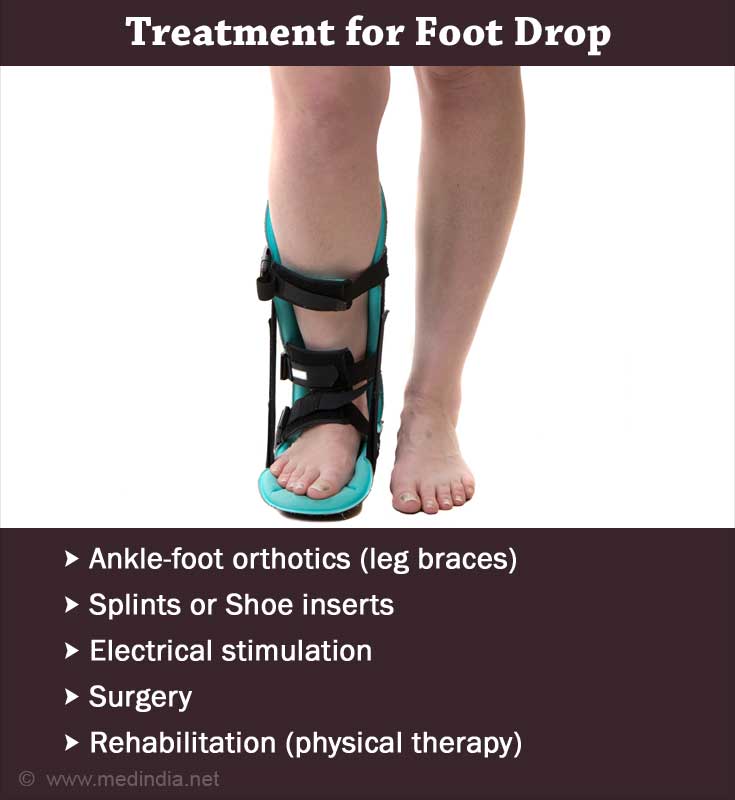
How can you Treat Foot Drop?
Treatment and its outcome usually revolve around treating the underlying cause. If there is severe damage to the extent where the pathology cannot be reverted, it may lead to a permanent foot drop. The common management strategies involve:
- Ankle-foot orthotics: A lightweight leg brace, usually made of plastic to support the foot.
- Splints or shoe inserts: Aids in supporting the foot in normal position.
- Functional electrical stimulation (FES): Electrical devices stimulate the peroneal nerve or affected nerves and muscles to improve foot drop. This may further reduce foot spasticity (tightness), strengthen the muscles, enhance the gait, walking, and balance.
- The Bioness L300 Foot Drop System: An electrical leg cuff worn just below the knee along with a gait sensor attached to the shoe for treating foot drop via electrical stimulation.
- Surgery:
- In case of any trauma, nerve reconstruction surgeries like autologous nerve grafts should be performed within 72 hours of injury.
- Surgical release procedure in patients with equinus deformity (inability to dorsiflex/lift the foot).
- Interventions that repair the foot and ankle joint by fusing them, e.g., Ankle Arthrodesis.
- Total knee replacement surgery in the event of partial peroneal nerve palsy.
- Tendon transfer – Transferring the tendons (connective tissue for joining the muscles to bones) from other stronger muscles (commonly posterior tibial tendon) is performed in severe cases.
- Bridle procedure – Involves transfer of all three tendons namely posterior tibial tendon (near the ankle), the peroneus longus (outer part of the lower leg), and the anterior tibialis (anterior side of the shin) for the repair of foot drop.
- Medications to relieve pain (gabapentin & duloxetine)
- Erythropoietin - An anti-inflammatory, neurotrophic hormone that aids in promoting repair of the damaged nerves.
- Rehabilitation: Physical therapy, stretching exercises, gait training, and guided foot drop exercises help strengthen the leg muscles to further improve joint movement, balance, and gait. Certain exercises that may be done for enhancing the recovery are:
- Ball Lift
- Toe-to-Heel Rocks
- Towel Stretch
- Ankle Dorsiflexion
- Plantar Flexion
- Marble Pickup
Prognosis of Foot Drop
The prognosis is more likely to be good with partial or even complete recovery if the underlying disease is treated effectively.
- The recovery period of peripheral compressive neuropathy is up to 3 months.
- In case of damage to nerves, recovery may take up to 6 to 12 months
- However, in cases of progressive neurological disorders, foot drop may seem like a lifelong disability. This would further invite increased morbidity especially in the elderly due to recurrent falls.
What are the other Conditions that can Mimic Foot Drop?
- Upper motor neuron involvement like hemiparesis or hemiplegia in stroke
- Cerebellar gait – Walking deficits due to dysfunction of the cerebellum
- Ataxic gait as seen in alcohol abuse disorder
- Parkinsonian gait – A movement disorder that results in a short shuffling gait
- Lumbar plexus involvement
- Diabetic amyotrophy – Diabetes complication that results in muscle wasting
How to Prevent Foot Drop?
Certain measures that may be considered to reduce the added symptoms of foot drop like tripping or falling are the following:
- Ensure proper lighting in the rooms
- May consider fluorescent tape for staircase
- Secure clear pathways devoid of electrical cords and obstacles when walking on the floor
- Avoid tripping or slipping hazards nearby
- Continue physical exercises