- Wyndham, Christopher R.C. "Atrial Fibrillation: The Most Common Arrhythmia." Texas Heart Institute Journal 27.3 (2000): 257-267. Print.
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991 Aug;22(8):983-8. PubMed PMID: 1866765.
- Atrial fibrillation - (http://www.nhs.uk/conditions/atrial-fibrillation/pages/introduction.aspx)
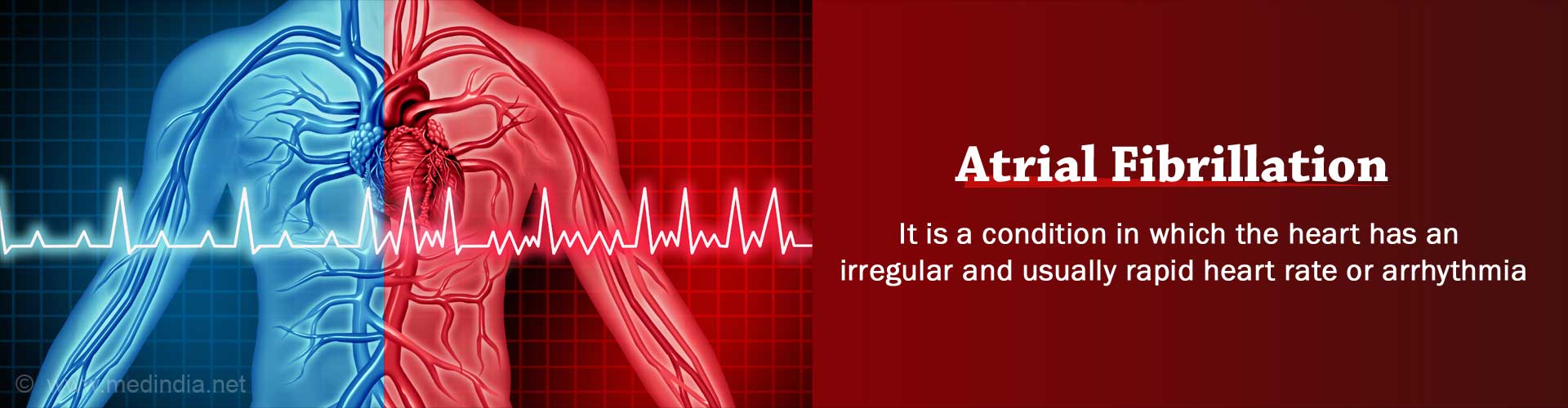
What is Atrial Fibrillation?
Atrial fibrillation is a condition in which the heart has an irregular and usually rapid heart rate or arrhythmia. This inhibits blood flow and circulation through the body, posing several health risks. Under normal circumstances the heart rate of a healthy individual at rest should be 60 to 100 beats a minute. If you suffer from atrial fibrillation however, the heart rate could be well over 140 beats per minute. The main difference however is not just the accelerated heart rate, but its irregularity.
Atrial fibrillation may arise as a temporary problem that comes and goes, but it could also be persistent in other cases and would require treatment. The condition may not pose any direct threat to your life but it can increase the risk of various life-threatening conditions. It should always be treated as a serious medical condition and in some situations, emergency treatment may actually be necessary.
Atrial fibrillation is classified into different types, depending on the extent to which it affects you:
Paroxysmal atrial fibrillation – This refers to cases where the atrial fibrillation is episodic. The condition comes and goes of its own accord without any intervention, but treatment can be used to stop an episode as soon as it begins.
Persistent atrial fibrillation – This type of atrial fibrillation lasts for over a week and is unlikely to resolve without treatment. Treatment can help to restore normal heart rhythm, but the condition can recur at a later point.
Permanent atrial fibrillation - Atrial fibrillation cannot be resolved completely. Treatment may have been tried to restore normal heart beat but have been unsuccessful. The main aim when dealing with permanent atrial fibrillation is to lower the heart rate, so that it is in or is closer to the normal range, but the rhythm remains irregular.
What are the Causes of Atrial Fibrillation?
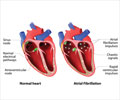
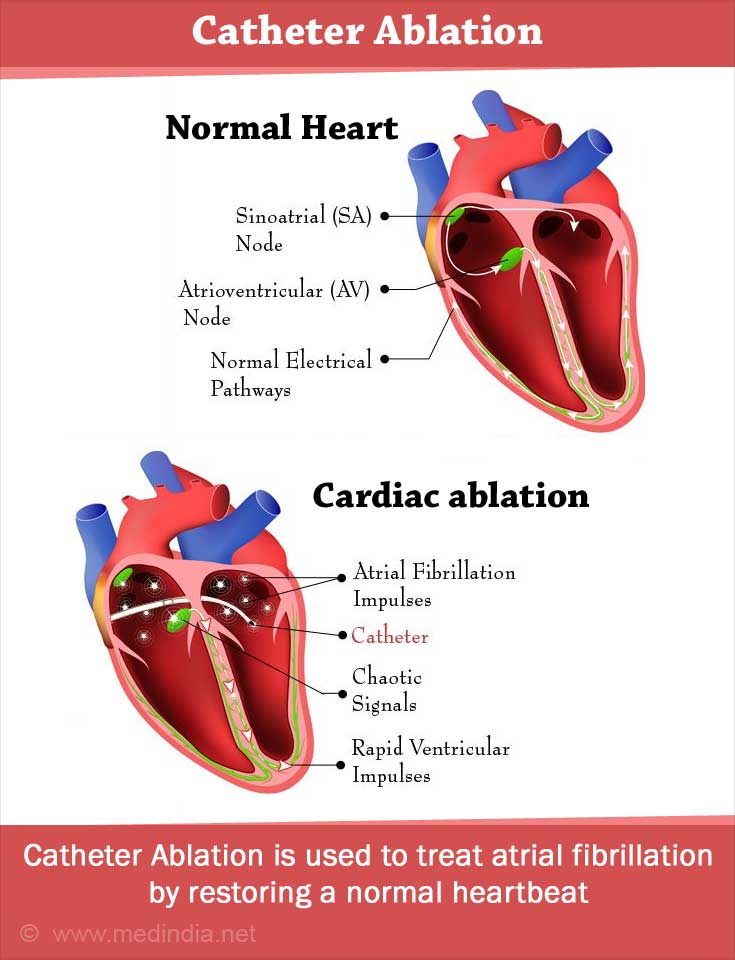
To understand the causes of atrial fibrillation it is important to understand how the heart normally functions. The heart comprises of four chambers, with two upper chambers called atria and two lower chambers called ventricles. The heart has a natural pacemaker that regulates heart beat rhythm and this group of cells, which is located in the upper right chamber of the heart, is called the sinus node. The sinus node produces electrical impulses that travel first through the atria and then through the ventricles below. These impulses signal the start of each heartbeat and regulate the flow of blood through the contractions of the heart muscles. The atria contract and pump blood to the ventricles, then the ventricles contract, pumping blood through the body. These impulses from the sinus node travel are transmitted from the atria to the ventricles through a pathway called the atrioventricular (AV) node.
When atrial fibrillation is present there is a problem with these electrical signals, with the atria receiving chaotic impulses. This causes a quiver and a very rapid heartbeat in the atria. All of these impulses that cause the quiver and accelerated heartbeat cannot reach the ventricles however, as the AV node cannot convey this surge of impulses. As a result, the ventricles also experience an increased beat, but not as dramatic an increase as the atria. This combination produces an irregular but fast heart rhythm. While the normal range heart rate is 60 to 100 beats per minute, this condition can cause the rate to be in the range of 100 to over 200 beats per minute.
Possible causes and risk factors for atrial fibrillation include:
- Hypertension is the most frequent cause of the condition because of the increased strain that the heart muscle is subjected to.
- Atrial fibrillation often develops as a complication of other kinds of heart conditions like ischaemic heart disease, dilated and hypertrophic cardiomyopathy, pericardial disease and heart valve problems.
- Conditions like pulmonary embolus, pneumonia, diabetes, hyperthyroidism and lung cancer.
- Obesity also increases the risk of atrial fibrillation.
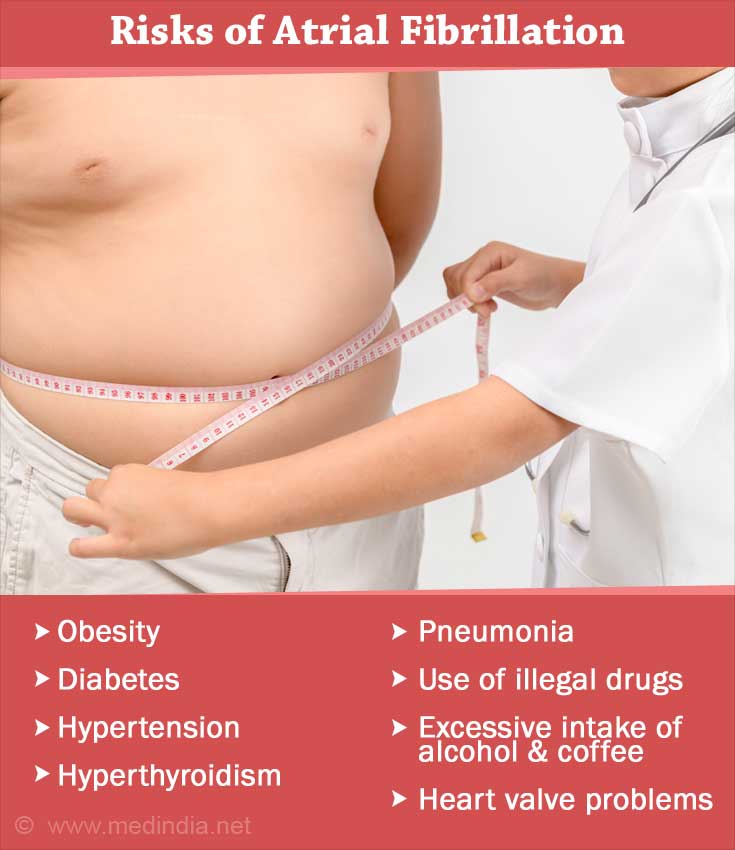
- The excessive intake of both alcohol and caffeine.
- The consumption of illegal drugs like amphetamines and cocaine.
In some instances, patients may have what is described as lone AF. This accounts for about one out of ten cases, in which there is no known cause as the heart is otherwise healthy.
What are the Symptoms of Atrial Fibrillation?
There is a rapid onset of symptoms once the condition develops. These include:
- Breathlessness – This is the most common and usually the first symptom to be noticed. While the symptom could be present at any time it tends to be more pronounced and surfaces with any exertion.
- Heart palpitations – You may be conscious of your heart beat and notice an accelerated and irregular rhythm.
- Angina – Chest pain may surface when you exert or are stressed, but this could also occur when resting.
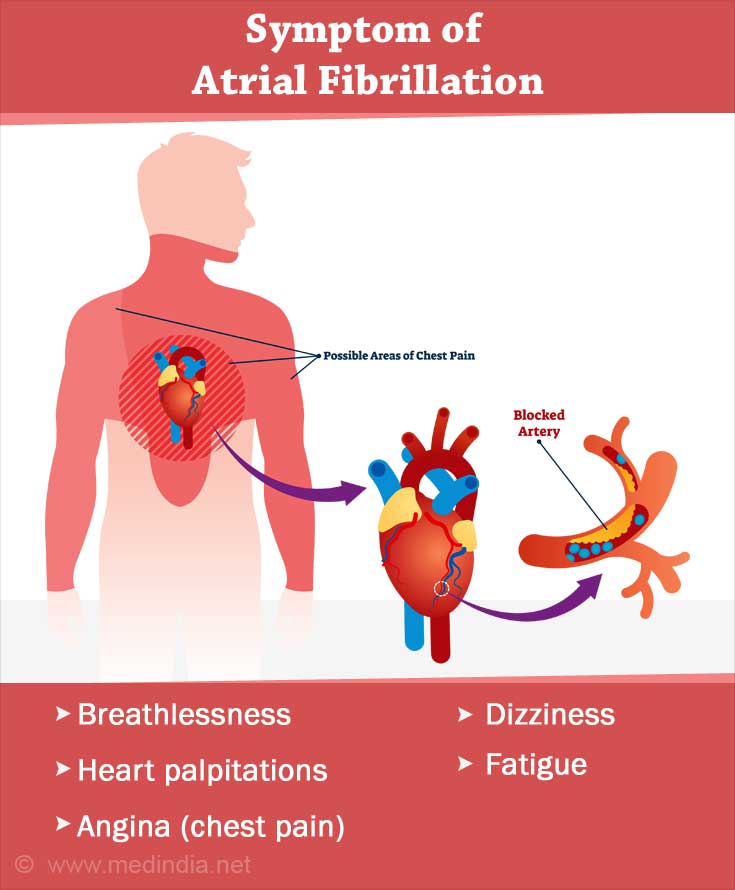
- Dizziness and fatigue.
Apart from heart palpitations, other atrial fibrillation symptoms tend to surface because of reduced efficiency of the heart, as smaller amounts of blood are pumped through the body at a greater rate. If the heart rate is not significantly higher than normal the condition may not even cause any symptoms and will only be picked up during routine health checks.
How to Diagnose Atrial Fibrillation?
While you can check your pulse rate at home yourself, this alone cannot be used as conclusive evidence for atrial fibrillation. Make it a point to visit your doctor right away if you notice any irregularities or an elevated rate. Your doctor will need to review your medical history and will also have to be informed about any symptoms that might be present. In addition to a physical examination your doctor will also recommend certain tests to help make a diagnosis.
- An electrocardiogram or ECG is the most effective and commonly used method of testing for atrial fibrillation. It is a tool that tracks and monitors the electrical activity of your heart.
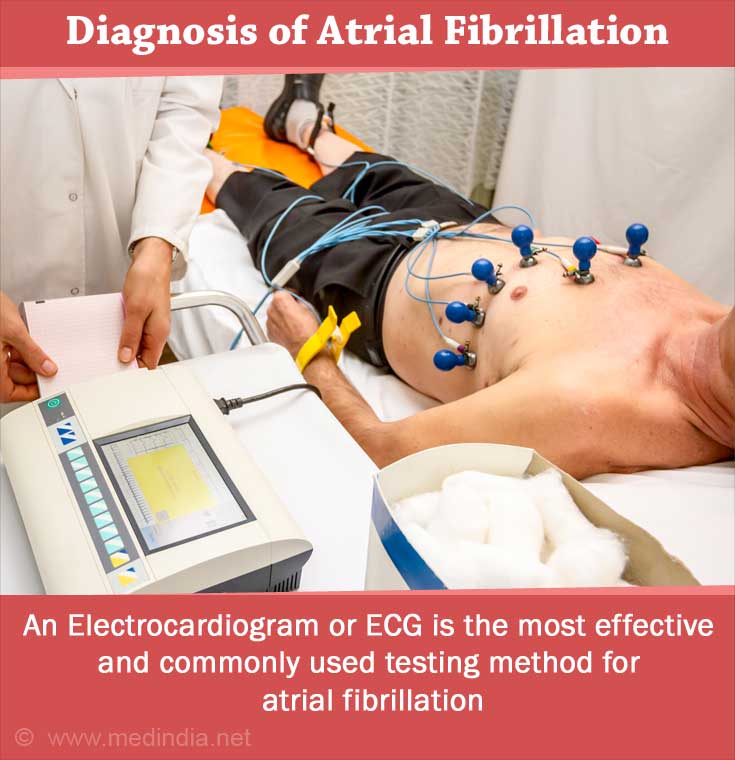
- Paroxysmal atrial fibrillation can be a bit harder to diagnose and your heart rhythm would need to be recorded for a longer duration. This would require the use of diagnostic tools like ambulatory EKG and Holter monitoring, which enable portable monitoring of your heart rate and rhythm.
- Blood tests to check for conditions like hyperthyroidism.
- Prothrombin time and INR to check blood clotting time if you are on blood thinning medications like warfarin.
Other tests that could be recommended include electrophysiology and echocardiogram.
What are the Treatments for Atrial Fibrillation?
Treatment for atrial fibrillation will differ from patient to patient. Health care specialists treat the condition based on symptoms and other factors after carefully evaluating other health risks. The main aim of treatment is to provide relief from the symptoms and prevent a recurrence of the condition, and most importantly to lower the risk of complications like strokes and heart failure.
Based on these considerations, treatments follow three approaches.
Treatment to slow the heart rate
Treatment to slow heart rate involves the use of rate-control medicines that can help to control your heart rate. While they will help to prevent a dangerously fast rate, they cannot regularize the heart rhythm itself. This alone can help to improve the efficiency of the heart, however. This line of treatment is usually very effective although dosage and drug combinations will differ and need to be altered for different patients. Medications that are used to slow the heart rate include beta-blocker medicines, calcium-channel blocker medicines and digoxin.
Treatment to regulate and regularize heart rhythm
This includes and refers to treatments that are used to restore a normal heart rhythm and stop atrial fibrillation altogether. Prevention of recurrence is also an important aspect of this treatment. This approach involves the use of:
- Antiarrhythmics or rhythm-control medicines
- Electrical cardioversion, which is a procedure in which low-voltage electrical shocks are used to restore a normal rhythmic heartbeat. The use of cardioversion for atrial fibrillation is limited in its scope however as it is not recommended in certain situations and its effects are often temporary and atrial fibrillation returns within a year.
- Catheter ablation is usually used as a treatment when medications fail to restore a normal heartbeat or if the side effects of medications are too severe. This is because the treatment doesn’t always work and atrial fibrillation ablation also poses a risk of serious complications.
- Maze procedure is a technique that uses scarring to restrict electrical impulses that trigger the problem of atrial fibrillation. The procedure is typically carried out in open-heart surgery, with scar tissue being created to block and filter the excessive and chaotic impulses.
Preventive treatment for strokes
When the heart contracts inefficiently due to atrial fibrilation, blood clots can form in the heart because of sluggish flow and these blood clots can travel to the lungs accusing pulmonary embolus or to the brain causing stroke. Both pulmonary embolus and stroke are potentially fatal, so treatment to prevent these complications is absolutely essential. Doctors typically recommend the use of anticoagulant medications to reduce the risk of pulmonary embolus or stroke. Anticoagulants or (“blood thinners”) interfere with the action of certain proteins in blood to prevent the formation and propagation of blood clots. Anticoagulants reduce the risk of pulmonary embolus and stroke considerably, but they pose some risks of bleeding if too much drug is present in the body. If patients are on Coumadin, it is important to regularly test blood clotting time using the International Normalized Ration (“INR”) blood tests. Newer anticoagulant drugs are safer to use because of their decreased bleeding risk
What are the Complication and Risks of Atrial Fibrillation?
The highest risk posed by atrial fibrillation is the risk of stroke. This is because there is high risk of blood clot formation in the atria because of the inefficient pumping of blood. Such blood clots can travel to the lower chambers of the heart from where they can be pumped along with the blood supply to any part of the body. Such blood clots will travel in blood vessels until it gets stuck or lodged in a smaller blood vessel or in an organ like the lungs or brain. When the clot gets stuck in a blood vessel in the brain it blocks or reduces blood flow to the brain, thereby causing a stroke.
- The risk of a stroke is four to five times higher in patients suffering from atrial fibrillation. The extent of the risk posed is influenced by several factors and your doctor will take all of this into account before deciding on the course of treatment.
- Atrial fibrillation does put your heart under a great deal of pressure as it is forced to pump blood at an increased rate. This will eventually weaken the heart and in extreme cases can lead to heart failure.
- Similarly, weakness of the heart muscles or dilated cardiomyopathy is not uncommon in some patients suffering from atrial fibrillation.