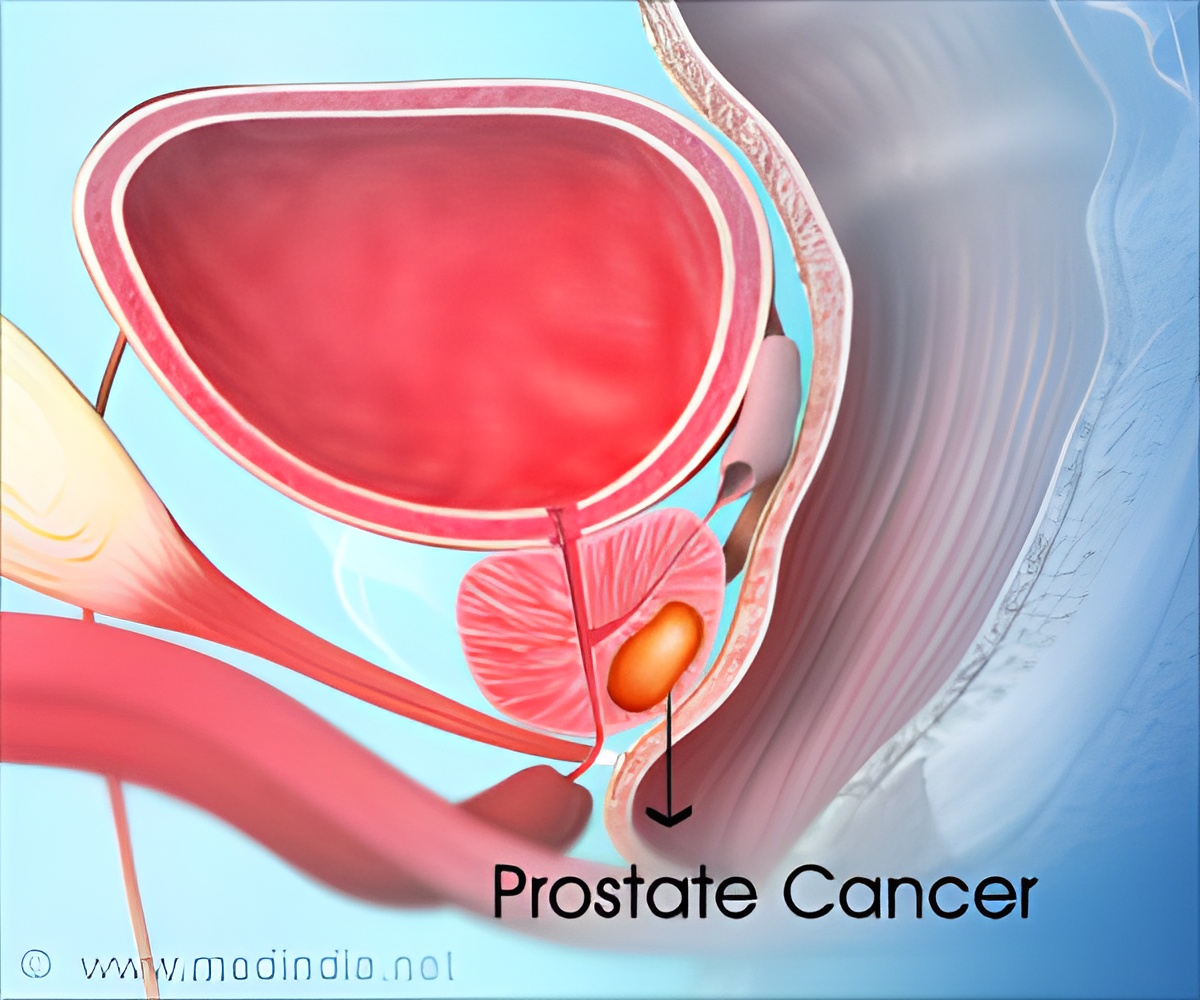
New imaging technology is less accurate than MRI at detecting prostate cancer.
TOP INSIGHT
MRI scan was far superior in the detection of any prostate cancer than the prostate-specific -PSMA PET/CT scanning technique.
The PrEscription of intraDialytic exercise to improve quAlity of Life (PEDAL) trial recruited 240 patients across five hospital groups who were at risk of prostate cancer. Every patient was given both an MRI scan and a PSMA PET/CT scan. If imaging suggested the presence of prostate cancer, a biopsy was performed by the patient’s urologist.
The MRI scans picked up abnormalities in 141 patients, while the PSMA PET/CT scans picked up abnormalities in 198 patients. A total of 181 patients (75%) underwent a prostate biopsy, and subsequently, 82 of those patients were found to have clinically significant prostate cancer.
Since each patient had both types of scans, the researchers could assess which type had more accurately detected those patients who had prostate cancer. The researchers found that MRI scans were significantly more accurate at detecting prostate cancer grade than the PSMA PET scans (0.75% for MRI vs 0.62% for PSMA PET).
Associate Professor Lih-Ming Wong, Consultant Uro-oncologist at St Vincent’s Hospital in Melbourne, Australia, headed the research team. He said: “Our analysis found that MRI scans were better than PSMA-PET for detecting any prostate cancer grade. When we looked only at clinically significant prostate cancers, there was no difference in accuracy. As this study is one of the first to explore using PSMA-PET to diagnose cancer within the prostate, we are still learning and adjusting how to improve using PSMA-PET in this setting.
He says: “This study confirms that the existing ‘gold standard’ of pre-biopsy detection – the MRI – is a high benchmark. Even with fine-tuning, we suspect PSMA PET/CT won’t replace the MRI as the main method of prostate cancer detection. But it will likely have application in the future as an adjunct to the MRI, for people for whom an MRI is unsuitable, or as a combined "diagnostic and staging” scan for appropriately selected patients.”
Professor Peter Albers, Chair of the European Association of Urology’s Chief Scientific Officer, comments: “New diagnostic tools need to be tested as carefully as new drugs, so we welcome the findings of this remarkable Phase III trial, which showed that MRI was superior in the detection of any prostate cancer.
“It also showed that PSMA PET/CT was not inferior to MRI in the detection of clinically significant cancers (ISUP 2 and higher); and since the ultimate goal of primary staging will be to detect only the more aggressive cancers and avoid unnecessary biopsy, this is not the end of the story. More research will be needed to explore the PSMA PET/CT correlation between the standard uptake value (SUV) and cancer aggressiveness, but the first steps down the road in finding the best diagnostic approach to clinically significant prostate cancer have been taken.”
Source-Eurekalert
 MEDINDIA
MEDINDIA



 Email
Email



![Prostate Specific Antigen [PSA] Prostate Specific Antigen [PSA]](https://www.medindia.net/images/common/patientinfo/120_100/prostate-specific-antigen.jpg)




