Targeted gene therapy destroys herpesvirus-linked cancer cells while protecting healthy tissue, offering safer treatment.

Design, development, and evaluation of gene therapeutics specific to KSHV-associated diseases
Go to source).
TOP INSIGHT
A promising new #genetherapy is targeting #Kaposi_sarcoma and related conditions driven by the KSHV (Kaposi's sarcoma–associated herpesvirus). The virus-driven cancer remains a major global health concern, especially for those with weakened immune systems. #KSHV #CancerResearch #GlobalHealth #HIV
Advancing Cancer Treatment: A Safer, More Specific Gene Therapy Approach
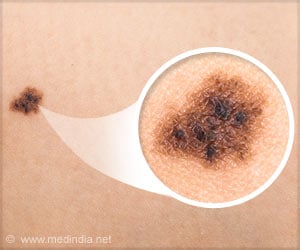
This innovative approach shows the potential to transform treatment by attacking cancer cells with high specificity while minimizing harmful side effects that often come with conventional therapies. Researchers believe the therapy represents a significant step forward in advancing safer, more effective options for patients.The therapy is aimed at Kaposi’s sarcoma and related conditions caused by the Kaposi’s sarcoma–associated herpesvirus (KSHV). This virus-driven cancer remains a major global health concern, particularly among individuals with weakened immune systems, such as people living with HIV/AIDS in regions like sub-Saharan Africa.
By addressing the underlying viral cause, the UC Davis team hopes to open new possibilities for treating these difficult-to-manage cancers, improving outcomes for vulnerable populations worldwide.
Findings from the research are now published and will appear in the December issue of Molecular Therapy Oncology. The study’s lead author is Yoshihiro Izumiya, a professor in the UC Davis Department of Biochemistry and Molecular Medicine and the Department of Dermatology.
“The new strategy uses a specialized gene therapy technique to selectively target and kill cancer cells infected with the virus — while leaving healthy cells unharmed,” Izumiya said.
Izumiya and members of his lab at UC Davis performed their research using mouse models. “The treatment significantly reduced tumor growth with no detectable side effects,” Izumiya said.
The therapy harnesses a harmless virus called adeno-associated virus (AAV) to deliver a genetic “Trojan horse” into infected cells. It does so by using the virus’ own protein to drive the therapeutic agents into the cancer cells to kill the cells.
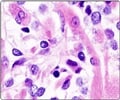
This gene therapy is designed to become active only in cells harboring KSHV, thanks to a viral marker protein known as LANA, which is only found in KSHV-infected cancer cells.
Harnessing a "Trojan Horse": AAV Gene Therapy for Selective Cancer Cell Destruction
Once inside the KSHV-infected cell, the therapy delivers a gene for a modified thymidine kinase enzyme that converts a common anti-herpesvirus drug — ganciclovir — into a cancer-killing agent. When the drug is added, only the infected cells are affected, triggering their death while sparing healthy tissue.“This is a precision-guided approach that uses the virus’s own tricks against it,” said Izumiya. “It’s like delivering a self-destruct signal directly into the cancer cells.”
In tests with lab-grown human cells, the therapy successfully eliminated KSHV-infected cells while leaving uninfected ones unharmed. When tested in mice with KSHV-related tumors, the therapy — combined with ganciclovir — effectively halted tumor growth.
Importantly, the treatment caused no observable side effects in mice, suggesting a high level of safety.
Researchers also discovered that anti-cancer drugs known to reactivate KSHV made the therapy even more effective, boosting its impact by enhancing the delivery system's activation.
The Challenge of KSHV-Linked Cancers
KSHV is responsible for several aggressive cancers, including Kaposi’s sarcoma and two rare lymphomas. While current treatments exist, they often come with significant side effects and are not always effective, especially in immunocompromised patients.This new gene therapy could offer a safer, more targeted option. By focusing only on virus-infected cells, the treatment minimizes the risk to healthy tissues — a major hurdle in conventional cancer therapy.
This research is still in its early stages and will require further testing before it can move to human trials. But the results offer hope for a more precise, less toxic way to treat KSHV-related cancers and possibly other cancers caused by viruses.
“Our goal is to turn the virus’s own biology into its weakness,” Izumiya said. “This is a step toward smarter, more personalized cancer treatments.”
Reference:
- Design, development, and evaluation of gene therapeutics specific to KSHV-associated diseases - (https://www.cell.com/molecular-therapy-family/oncology/fulltext/S2950-3299(25)00119-5)
Source-Eurekalert
 MEDINDIA
MEDINDIA



 Email
Email