- Molluscum contagiosum - Mayo Clinic - (https://www.mayoclinic.org/diseases-conditions/molluscum-contagiosum/diagnosis-treatment/drc-20375230)
- Molluscum contagiosum - Centers for Disease Control and Prevention (CDC), USA - (https://www.cdc.gov/poxvirus/molluscum-contagiosum/index.html)
- Molluscum contagiosum - American Academy of Dermatology - (https://www.aad.org/public/diseases/contagious-skin-diseases/molluscum-contagiosum)
- Olsen JR, Gallacher J, Piguet V, Francis NA. Epidemiology of molluscum contagiosum in children: a systematic review. Fam Pract. 2014 Apr; 31(2): 130-6. DOI: 10.1093/fampra/cmt075 . PMID: 24297468.
- Hay RJ, Johns NE, Williams HC, Bolliger IW, Dellavalle RP, Margolis DJ. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014 Jun; 134(6): 1527-34.
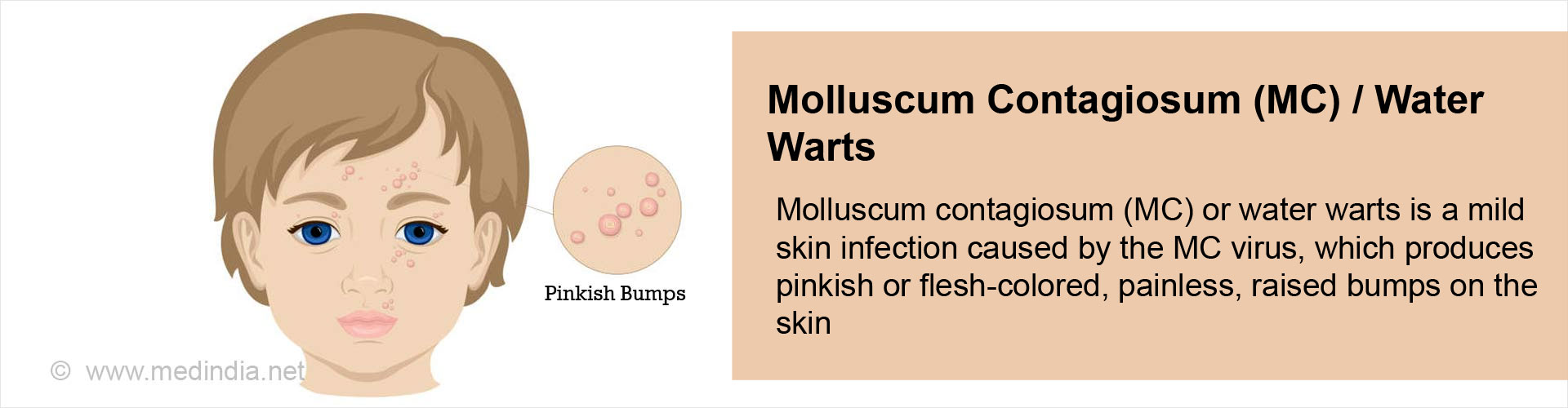
What is Molluscum Contagiosum?
In the year 2010, almost 1.8% of the world population or 120 million were affected by a harmless skin infection called molluscum contagiosum (MC) or water warts. The condition is caused by the molluscum contagiosum virus (MCV) which belongs to the family of poxviruses. The infection is characterized by pinkish or flesh-colored raised bumps on the skin and generally it disappears without medical treatment within a year.
The bumps can occur anywhere in the body, but are most common on the face, neck, arms, legs, armpits, groin as well as the trunk of the body. The number of bumps often depends on the immune status of the patient. Individuals with a weak immune system often have larger number of bumps and vice versa. The virus infection spreads either by direct skin-to-skin contact or via fomites, such as contaminated towels, clothes or other objects. The infection causes no scarring. As this is a harmless lesion, a child can continue to attend school or daycare.
Epidemiology of Molluscum Contagiosum
The incidence rate is around 12-14 episodes per 1000 children per year. There is a higher incidence in warm, tropical climates and it is more commonly associated with poor hygiene. Although MC infections can occur at any age, they are most common in young children between 1-10 years of age, which accounts for roughly 80% of the cases.
What are the Types of Molluscum Contagiosum?
Molluscum contagiosum is of three types, based upon the three stages through which the infection passes. These include the following:
- Stage 1: This initial stage is characterized by the appearance of small whitish, pinkish or reddish bumps on the skin.
- Stage 2: During this stage the bumps enlarge to about 2-5 mm in diameter and become filled with white pus. This is followed by rupturing, which leaves a crater at the center of the lesion.
- Stage 3: In this final stage, the craters develop into red sores. These open sores may lead to secondary infections, especially bacterial infections, which may require treatment with antibiotics.
What are the Causes of Molluscum Contagiosum?
Molluscum contagiosum is caused by MCV infection, which can spread in the following ways:
- Direct Skin-to-Skin Contact: The disease can spread from person-to-person by touching an infected person.
- Fomites: The disease can be spread by coming in contact with fomites such as infected clothing, towels, bathing sponges, utensils, toys, and other objects that can harbor the virus and transmit it by touching.
- Sexual Contact: The disease can be spread by intimate physical contact as well as through sexual intercourse with an infected person. For this reason, MC is also considered as a sexually transmitted infection (STI).

What are the Symptoms and Signs of Molluscum Contagiosum?
The primary symptom of MC is the appearance of bumps on the skin, often exhibiting the following signs:
- Small (<6 mm), round, raised, painless
- Pink or flesh colored
- Small indentation in the center
- Can become red, inflamed, and itchy
- Highly contagious
- Present on face, neck, armpits, abdomen, arms, and back of the hands in children
- In adults, all of the above, as well as the genitals and upper thighs in case of sexual contact
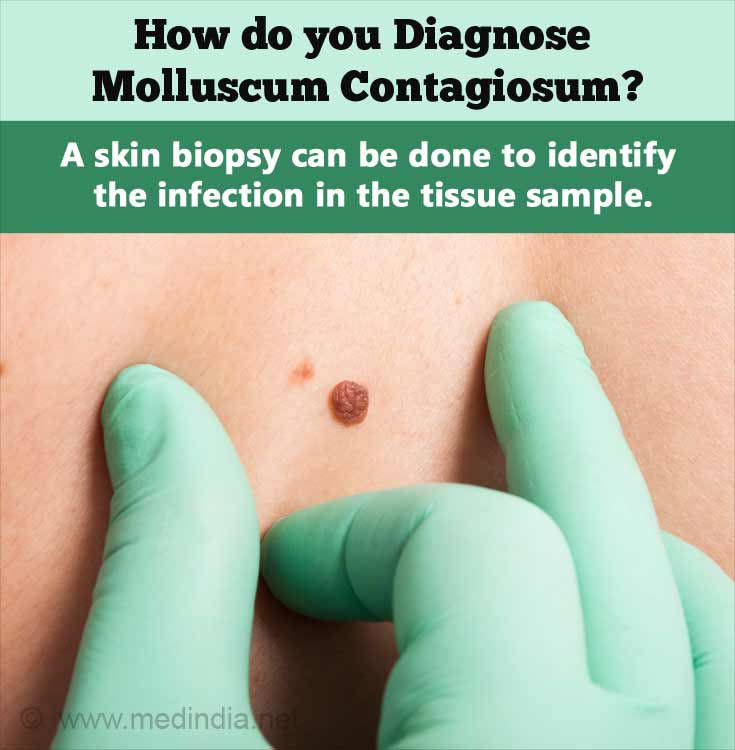
How do you Diagnose Molluscum Contagiosum?
- Clinical Examination: Diagnosis is generally established just by looking at the bumps. An experienced dermatologist can easily diagnose the condition by a simple clinical examination.
Skin Biopsy : If in doubt, a skin biopsy can be done to identify MCV in the tissue sample by microscopy. This is the definitive diagnosis for MC.
How do you Treat Molluscum Contagiosum?
Treatment for MCV infections are generally not recommended, especially for children as the symptoms generally resolve by itself (usually within a year) and the infection does not interfere with daily activities. However, there are several treatment options that are available for adults in whom the disagreeable appearance may interfere with the nature of their occupations e.g. celebrities like actors and other public figures. These treatment options are briefly discussed below:
- Topical Medications: Medicated creams or gels may be applied to the skin to resolve MC lesions. The drugs that are used in these creams or gels include tretinoin, tazarotene, and adapalene. However, these medicines cannot be used in pregnant women. Imiquimod and podophyllotoxin creams have also been recommended for treating MC.
- Oral Medication: Cimetidine is an oral drug that is recommended, especially for children, who cannot withstand the discomfort from physical treatment methods.
- Keratolytic Agents: These include creams containing a keratolytic (skin peeling) agent such as salicylic acid, potassium hydroxide or trichloroacetic acid that help to resolve the lesion by peeling off the skin at the lesion site. Cantharidin, a blistering agent, has also been recommended for treating MC.
- Curettage: This term means “scraping”. In this procedure, the lesion is opened up and the inside is scraped out. However, scraping can result in scarring.
- Cryotherapy: This procedure uses liquid nitrogen to freeze the site of the lesion to lift off the affected skin.
- Laser Therapy: A special type of laser called pulsed dye laser (PDL) can be effectively used to resolve the lesions.
What are the Risk Factors for Molluscum Contagiosum?
There are several risk factors for MC, including the following:
- Weakened immune system e.g. HIV/AIDS patients
- Atopic dermatitis / eczema
- Crowded living conditions
- Using a communal bath or swimming pool
- Using steam baths and saunas
- Contact sports e.g. wrestling
- Athletes who share equipment e.g. gymnasts
What is the Prognosis of Molluscum Contagiosum?
The prognosis or outlook of MC after treatment is generally excellent. Moreover, the infection generally resolves by itself within a year, even without treatment. However, sometimes complications may arise such as secondary bacterial infections, including that of the eyes, causing conjunctivitis or keratitis. Immunocompromised patients are especially prone to developing secondary infections, resulting in poor prognosis.