- Liver and Bile Duct Cancer�Patient Version - (https://www.cancer.gov/types/liver)
- About Liver Cancer - (https://www.mdanderson.org/cancer-types/liver-cancer.html)
- Liver Cancer Treatment - (http://www.mayoclinic.org/diseases-conditions/liver-cancer/diagnosis-treatment/treatment/txc-20198180)
- Treatment of Liver Cancer - (https://en.wikipedia.org/wiki/liver_cancer)
- Chemoembolization - (http://www.radiologyinfo.org/en/info.cfm?pg=chemoembol)
- Hepatocellular carcinoma - (https://medlineplus.gov/livercancer.html#cat78)
- Cancer Immunotherapy - (http://www.cancerresearch.org/cancer-immunotherapy/impacting-all-cancers/liver-cancer)
- Liver Cancer - (http://www.cancer.org/cancer/livercancer/index)
- Maher JJ1. Exploring alcohol's effects on liver function. Alcohol Health Res World. 1997;21(1):5-12. - ( https://pubmed.ncbi.nlm.nih.gov/15706758/)
- Epidemiology of hepatocellular carcinoma in India - (https://pubmed.ncbi.nlm.nih.gov/25755607/)
- Liver Cancer(Archived) - (https://www.ncbi.nlm.nih.gov/books/NBK448337/)
- Chemical Risk Factors of Primary Liver Cancer: An Update - (https://pmc.ncbi.nlm.nih.gov/articles/PMC7801911/)
- The liver - (https://pmc.ncbi.nlm.nih.gov/articles/PMC5897118/)
What is Liver Cancer?
Liver cancer, also known as hepatic cancer is an abnormal growth of cells in the liver. The leading cause of the disease is cirrhosis or scarring of the liver tissue.
What is the Function of the Liver?
To understand about liver cancer, we need to know more about the structure and function of the liver.

The liver is the largest organ present inside the body and is situated just below the right lung and the diaphragm. The liver lies close to the colon, the intestines and the right kidney. It roughly weighs about 1.5 kg and is deep red in color due to a rich blood supply. The liver performs several important functions:
- It plays a major role in the metabolic process and subsequently in the absorption of nutrients.
- It secretes a substance called bile, necessary for the breakdown of bigger fat molecules into smaller forms. The bile reaches the small intestine through the bile duct during the digestive process.
- It also stores various nutrients such as fats, carbohydrates, proteins and vitamins (Vitamin A and Vitamin B12).
- It produces substances required for clotting of blood. If not for the presence of these substances, even a minor injury could cause a lot of bleeding.
- It also plays an important role in the detoxification process and clears the body of harmful substances.
- It synthesizes proteins produces cholesterol regulates amino acids.
What are the Types of Liver Cancer?
Liver cancer can be classified into two major categories, primary and secondary liver cancer.
1. Primary liver cancer originates from the cells present in the liver and is more common among middle-aged men and aged individuals (above 60 years of age). It can be differentiated into two major categories, depending on the origin of the tumor.
Hepatoma or hepatocellular carcinoma (HCC) originates from cells called hepatocytes that perform a majority of the liver function. It accounts for 75% of all primary liver cancers. It can occur as a single tumor and can spread to other parts of the liver or as multiple tumors in the liver at the same time.
Intrahepatic Cholangiocarcinomas originate from the cells that line the bile ducts of the liver and account for 10 to 20% of all primary liver cancers. The bile duct carries the bile to the gall bladder. Inflammation of the bowel and parasitic infection of the liver (liver fluke) are believed to cause this type of cancer.
Liver cancer cells can spread to other parts of the body such as the bones or lungs. This phenomenon of spread of the tumor from one region to the other is called metastasis.
2. Secondary liver cancer is so termed because it originates in some other region of the body such as the colon, stomach, esophagus, pancreas, lung or breast and spreads to the liver. It is also termed liver metastasis. It may be present either when the original cancer was detected or can surface months or years after the primary tumor has been removed.
Interestingly, secondary cancers of liver are more common than primary cancers, since liver is a common site for metastases to occur from various organs.
What are the Stages of Liver Cancer?
Stage 1 - There is a single localized tumor (any size) present.
Stage 2 - There is either a single tumor (any size) that has grown into blood vessels or there are several 5 cm tumors.
Stage 3a - There is more than one tumor, with at least one tumor that is larger than 5 cm.
Stage 3b - Out of several tumors present, at least one is growing into a branch of a major vein of the liver called the portal or the hepatic vein.
Stage 3c - Either a tumor has grown into a nearby organ other than the gallbladder or into the outer covering of the liver.
Up until this stage the cancer has not spread to nearby lymph nodes or distant sites.
Stage 4a - The tumors can be of any given size and number and may have grown into blood vessels or nearby organs. While the cancer has spread to nearby lymph nodes it has not spread to distant sites.
Stage 4b - The tumors can be of any given size and number. The cancer has spread to other parts of the body while the nearby lymph nodes may or may not be involved.
Key Facts and Statistics for Liver Cancer
- Liver cancer is more common in countries of sub-Saharan Africa and Southeast Asia. It also happens to be the predominant cancer in these areas.
- 700,000 people are diagnosed with liver cancer every year in the world.
- Liver cancer accounts for 600,000 deaths worldwide every year.
- While liver cancer incidence has more than tripled since 1980 there has been a recent decrease in young adult rates.
- Death rates due to the disease have increased since 1980 (2.7% increase in annual deaths from 2003 to 2012).
- In the United States, the American Cancer Society estimates that in 2016, 39,230 new cases will be diagnosed and 27,170 deaths will occur due to primary liver cancer and intrahepatic duct cancer,
- The overall ratio of mortality to incidence is 0.95 manifesting a poor outlook for the disease
What are the Risk Factors and Causes for Liver Cancer?
In general, cancer is caused when a cell’s DNA is damaged. DNA changes can turn on oncogenes (genes that cause cells to grow and divide) or turn off tumor suppressor genes (genes that slow down cell division and cause cells to die at the right time).
Several of these genes have to change to render a particular cell cancerous.
While having the below risk factors can cause cancer, the mechanism by which they act is only partially understood.
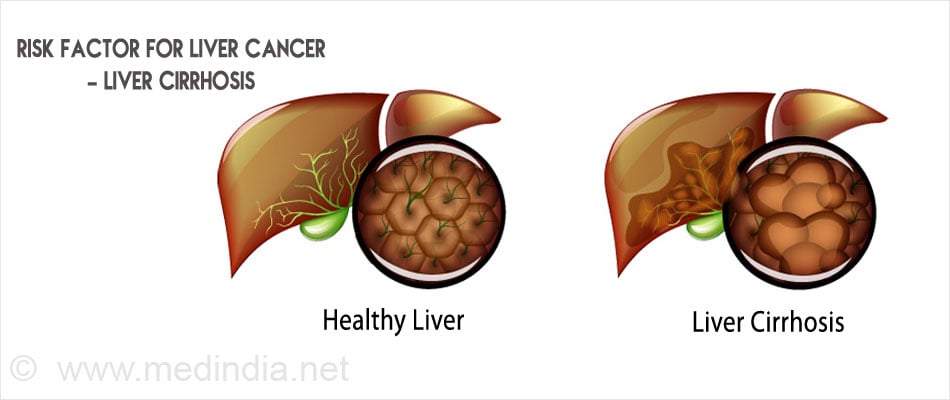
Cirrhosis of the Liver: Cirrhosis is a liver disease that occurs due to long-term damage to the liver as a result of alcohol consumption, viral infection (Hepatitis B and Hepatitis C) and genetic disorders like hemochromatosis and Wilson’s disease (characterized by excess build-up of iron and copper in liver tissues respectively). It can also be due to prolonged use of drugs or other chemical substances. The healthy liver cells get damaged over a long time and are replaced by scar tissue. About 5% of those with cirrhosis have chances of developing liver cancer (5%).
Hepatitis: Hepatitis is the medical term used to represent infection of the liver. Among the various agents that can give rise to infection, hepatitis C virus (HCV) and hepatitis B virus (HBV) deserve special mention.
The viruses can be passed on from one individual to another through sexual contact or blood and other body fluids. In addition, it may be passed on from an infected mother to her offspring.
It is hypothesized that the ability of the Hepatitis B virus to induce a genetic change in the normal liver cells (by insertion of the viral DNA into the DNA of the liver cell) could be responsible for causing liver cancer.
Hepatitis B infection can be prevented by active immunization through administration of the hepatitis B vaccine while a vaccine for hepatitis C is under experimental phase.
Alcohol Consumption: The liver is involved in the detoxification of substances such as alcohol from the body. Over consumption of alcohol causes an overload on the liver and damage occurs. Alcohol-related liver diseases like hepatitis, cirrhosis and fatty liver disease can also cause liver cancer.
The risk of developing cancer may be greater when there is a concomitant liver infection.
Aflatoxin Contamination: Aflatoxin B1, produced by a mold (Aspergillus flavus) has been known to have a strong association with respect to liver cancer. Storing of food such as peanuts, soybeans, corn, rice and wheat under hot and humid conditions can lead to aflatoxin contamination. This type of liver cancer is most common in China and Africa. Aflatoxin has been found to inactivate the tumor suppressor genes, eventually causing cancerous cells to grow.
Other risk factors include -
- Obesity - Obese people tend to develop non-alcoholic fatty liver disease called non-alcoholic steatohepatitis (NASH) and cirrhosis.
- Diabetes (High blood sugar)
- Primary biliary cirrhosis (PBC) - In this condition, bile ducts are destroyed causing cirrhosis. Advanced PBC increases the risk of liver cancer.
- Use of anabolic steroids by male athletes to increase strength and muscle mass.

- Drinking water containing arsenic.
- Family History - A person is more likely to develop liver cancer if he/she has other first-degree relatives afflicted with the same disease. This could probably be attributed to certain genetic factors that are shared between members of the same family.
- Gender - Men are twice as likely to develop HCC compared to women.
- Aflatoxin Exposure-Certain fungi on crops like corn and peanuts can produce toxic compounds that increase the risk of liver cancer.
What are the Symptoms of Liver Cancer?
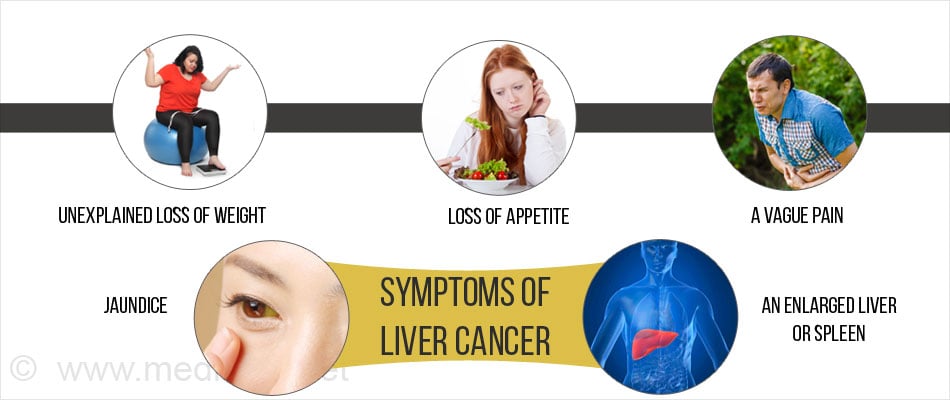
Symptoms are very rarely seen during the initial stages of liver cancer development. As the tumor progresses, it can lead to certain symptoms that can be experienced by the patient.
- Unexplained loss of weight
- Loss of appetite
- Generalized fatigue (common to all types of cancer)
- A vague pain, slight discomfort or a sensation of fullness may be felt in the upper abdominal area. The pain can also radiate to the right shoulder or to the back (enlargement of the liver affects the nerves that supply the area).
- Swelling/bloating of the abdomen due to fluid collection (ascites)
- Nausea and vomiting
- Jaundice (yellowish discoloration of the eyes and skin): if there is a block in the bile duct, the bile produced by the liver cannot reach the intestines or the gall bladder. It will then flow back into the blood, leading to the development of a yellow color in the skin and eyes. A patient with obstructive jaundice would also pass dark-colored urine and pale stools.
- An enlarged liver or spleen, felt as a mass under the ribs on the right side.
How is Liver Cancer Diagnosed?
Clinical Findings: An abdominal examination makes the doctor suspect liver cancer based on any change in the size or shape of the abdominal organs such as the liver, spleen or other neighboring organs. It can also reveal the presence of any abnormal fluid collection in the abdomen.
The skin and the whites of the eyes will also be checked for any yellow coloring or signs of jaundice.
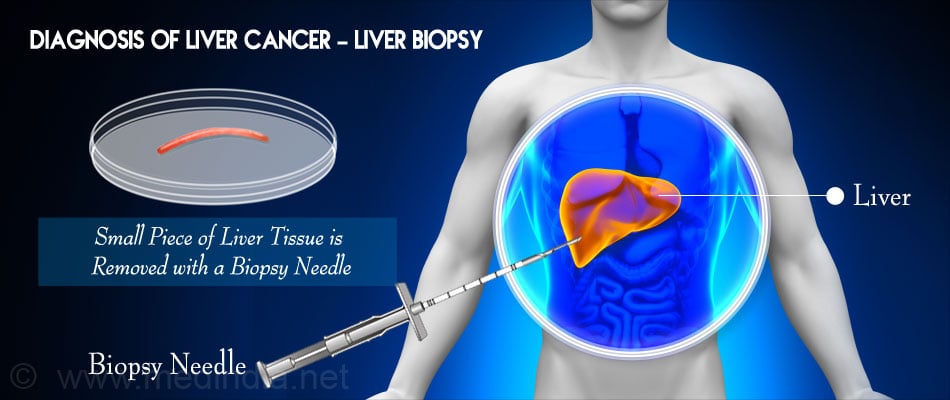
To confirm a diagnosis, blood tests, ultrasound tests, computed tomography (CT) scans, magnetic resonance imaging (MRI) and angiograms may be taken. A liver biopsy might also be ordered.
Blood Test: Blood tests can be used to provide information about functioning of the liver. A specialized test is the screening for alpha-fetoprotein, a tumor marker. It is a protein secreted by fetal liver. Soon after birth, the levels of this protein come down to normal levels.
Elevated levels of the protein are seen in liver cancer, ovarian and testicular tumors and when the tumor has spread from other organs to the liver. A level of AFP greater than 500 ng/ml is strongly suggestive of severe liver cancer. AFP level can also be used to determine the outcome of liver cancer treatment (it should decrease following successful surgical resection of the tumor).
Ascitic Fluid Analysis: Analysis of ascitic fluid and presence of cancer cells in the fluid points to a diagnosis of malignancy.
Ultrasound: It is usually the first imaging investigation ordered, as it is non-invasive, safe and relatively inexpensive, compared to the other methods. It can be used to assess the presence of the tumor, the number of tumors (single/multiple) or the extent of involvement of the neighboring structures and blood vessels. The amount of information obtained from an ultrasound examination is however, largely dependent on the skill of the person performing the same.
Computed Tomography: Serial cross-sectional images of the body are taken that help in the identification of the size, shape and position of the tumor in the liver. In order to obtain more information, a contrast material is given either through the mouth or through the intravenous route. If required, detailed information about the blood supply to and from the liver can be obtained.
Magnetic Resonance Imaging (MRI): Advanced forms of this imaging technique can provide a reconstruction of the images that would help the physician plan the treatment better. MRIs can help identify a benign tumor from a malignant one, assess the blood vessels in and around the liver and also indicate if the tumor has spread to other organs.
Angiography: A contrast agent is usually injected into a blood vessel and X-rays are taken. It shows the arteries that supply blood to the cancer and helps plan non-surgical treatments and operations.
Liver Biopsy: To determine the type of liver cancer, a thin needle is inserted through the skin surface to remove a small amount of the tissue. In some cases, the sample can be taken through ultrasound or CT guidance. It can also be removed when the patient is undergoing a surgery. The obtained sample is then sent to the pathologist who examines the tissue.
What is the Treatment for Liver Cancer?
Early detection and diagnosis of liver cancer is the key to successful treatment. The treatment outcome is much better if it is diagnosed before it has spread to other parts of the body. Surgery is one of the options available for treatment. However, the rest of the treatments are directed towards extending the lifespan and improving the quality of life of a liver cancer patient. A team of medical professionals (general surgeons, transplant surgeons, oncologists, radiotherapists, gastroenterologists) may participate in the treatment process.
Factors That Determine Treatment:
- Size, location and the number of tumors.
- Extent of liver damage and liver cirrhosis.
- Age and general health condition of the patient.
- Severity of the disease (spread to other parts of the body).
- Concerns regarding side effects of treatment.
Early-stage Treatment:
One of the following options is available if the liver’s function is preserved to an extent and the tumor is localized in a few easily accessible areas of the liver.
- Partial hepatectomy (removing a part of the liver) - A specific part of the liver that is affected by the tumor is removed by a process called liver resection. In some cases, removal of an entire lobe of the liver may be necessary.
The liver has an excellent regenerative capacity and the removed segment would be substituted by a new tissue within a few weeks or months.
- Liver transplantation (removal of the diseased liver and replacement with a healthy liver from a donor) is yet another option. It is usually performed for tumors that cannot be removed by surgery either due to its location or because the liver is too deceased. It is also used to treat small tumors that have not spread to the blood vessels.
- Tumor ablation is done when surgery is not an option. This destroys live tumors without destroying the healthy cells.
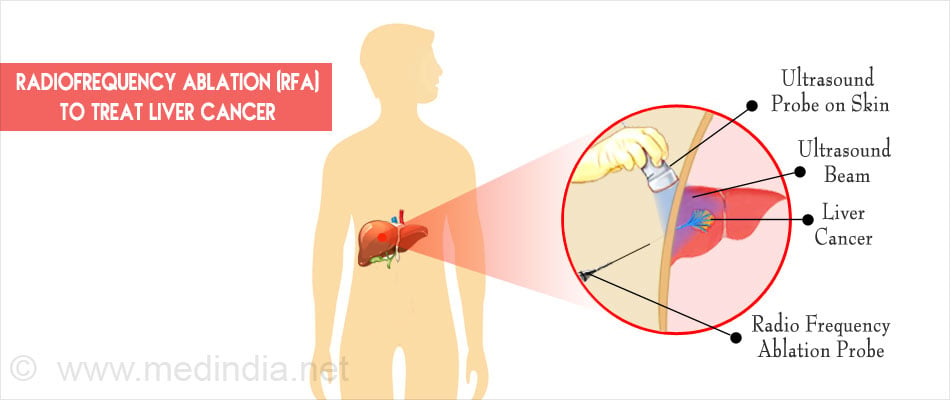
- Radiofrequency ablation (RFA) - Thin needles are inserted into the abdomen using an ultrasound or a CT scan. When the needles reach the tumor, they are heated with an electric current to destroy the cancer cells.
- Cryoablation - An instrument called a cryoprobe that contains liquid nitrogen is guided to the site of the tumors using ultrasound images. The cold temperature of the liquid nitrogen destroys cancer cells.
Advanced-stage Cancer:
Liver cancer cannot be removed if it has spread to other places such as the lungs or bones or the liver is extensively damaged as in cirrhosis. So when the cancer has corrupted multiple parts of the liver or has invaded the blood vessels or outside organs, treatment is usually aimed at prolonging life. Focus is also given on managing complications of liver cancer like pain, bleeding, obstruction of vital organs, blood clots and infection.
- Embolization is a technique that is aimed at cutting blood supply to the tumor. It is used for primary as well as metastatic liver cancer. 75% of the blood supply to the liver is through the portal vein and 25% is through the hepatic artery. Tumors in the liver get all their blood supply from the hepatic artery.
Medicines (transarterial chemoembolization or TACE) or radioactive microspheres (transarterial radioembolization or TARE) are injected directly into an artery leading to the liver to kill the cancerous cells. This is followed by sending embolic agents through the artery to block the blood supply to the tumors.
- Drugs that kill tumor cells like doxorubicin or cisplatin with lipiodol are used in chemoembolization.
- Chemotherapy (treatment by administering drugs orally or intravenously) usually does not give good results as the liver breaks down the drugs before they can reach cancer that is metastasized to other areas.
- Hepatic artery infusion: This procedure is used to infuse drugs continuously through a special implanted pump to a tube placed in the liver.
- Sorafenib is a targeted drug taken orally that works by blocking blood supply to the tumors and also targets some proteins and receptors that aid in cancer cell growth.
What are the Latest Developments in Treatment of Liver Cancer?
With our improved understanding of cancer biology, several new techniques are being developed to enhance the outcome of treatment. While such modalities are currently under the experimental phase, it promises a ray of endless hope in the cancer treatment. Some of these techniques are discussed below.
Magnetic Chemotherapy
Small magnets are attached to anti-tumor particles that are delivered to the tumor. A strong magnet is placed above the patient’s body and is positioned exactly over the tumor site. The delivered magnetic anti-tumor particles are then attracted to the exact site of the tumor owing to the presence of the strong magnetic field around the patient.
Gene Therapy
It is well known that tumors are caused due to subtle changes in small units that carry hereditary information from one generation to the other (gene). Active research is now being done to alter these defective genes and administer the corrected form of the gene to the patient in an attempt to treat the patient. It can be used for administration of specific drug formulations or cancer vaccines. The tumor can also be made more sensitive to either radiation or chemotherapy. This form of treatment is called gene therapy. Gene therapy has the potential to cure a patient of cancer.
What is the Prognosis for Liver Cancer?
Relative survival rates compare people with cancer to people in the overall population. A 5-year relative survival rate of 50% for a specific type and stage of cancer indicates that people in this category are 50% as likely to live for at least 5 years on average post diagnosis as those who do not have that cancer.
The 5-year relative survival rate for -
- Localized cancers are 30.5%
- Cancers spread to nearby organs and / or lymph nodes is 10.7%
- Cancers spread to distant organs and tissues is 3.1%
Surgeries like liver transplants can cure the patient of the cancer when it is localized. However to acquire a donor liver is a time-testing process and eventually only a small percentage of people get it. Surgical resections are successful in only one of three patients undergoing it.
How do you Prevent Liver Cancer?
Primary prevention (aimed at reducing exposure to a risk factor) can be accomplished by -
- Promotion of safe injection practice, screening of blood donation products and screening of high risk asymptomatic individuals thus controlling hepatitis infections.
- Vaccinations against hepatitis B infection.
- Post-harvest intervention to discourage mold thus preventing aflatoxin contamination.
- Reducing alcohol abuse, obesity and diabetes.

- Diet control (in hemochromatosis and Wilson’s disease).
Secondary prevention is achieved by treating diseases that could lead to liver cancer. For example hepatitis infections with antiviral drugs and aflatoxin contamination with chlorophyllin.
Tertiary prevention will prevent the cancer from recurring by putting the patient on post-operative chemotherapy and antiviral drugs.
Follow-up and Care of Patient after Initial Treatment
- After treatment has been completed, follow-up appointments are a must. If any problems persist, the doctor might ask for a blood retest or an imaging retest.
- If surgical resection or a transplant has been done and there are no signs of cancer remaining, imaging and blood tests have to be done every 3 to 6 months for the first 2 years and then every 6-12 months.
- Liver transplant patients also have to be monitored for rejections and other infections they might get due to being on immunosuppressant drugs.
- Patients who have acquired liver cancer due to hepatitis B or C infections have to be given antiviral drugs.
- In general, periodical follow-up tests and exams have to be done post-treatment including detection tests that detect the presence of other cancers.
- Refraining from smoking, drinking and eating healthy is important especially in the case of liver cancer as the organ is the seat of metabolism.
- For those who have advanced liver cancer, options they can choose from are enrolling in clinical trials that test new drugs or getting palliative care that provides relief from the symptoms, pain and stress of the disease.
- Some alternate ways to relieve pain are acupressure / acupuncture, deep breathing, listening to music as a therapy and massages.

 MEDINDIA
MEDINDIA
 Email
Email