Patients treated in Europe or Asia were 2.6 times as likely to undergo breast conserving therapy rather than a mastectomy, found new study.
TOP INSIGHT
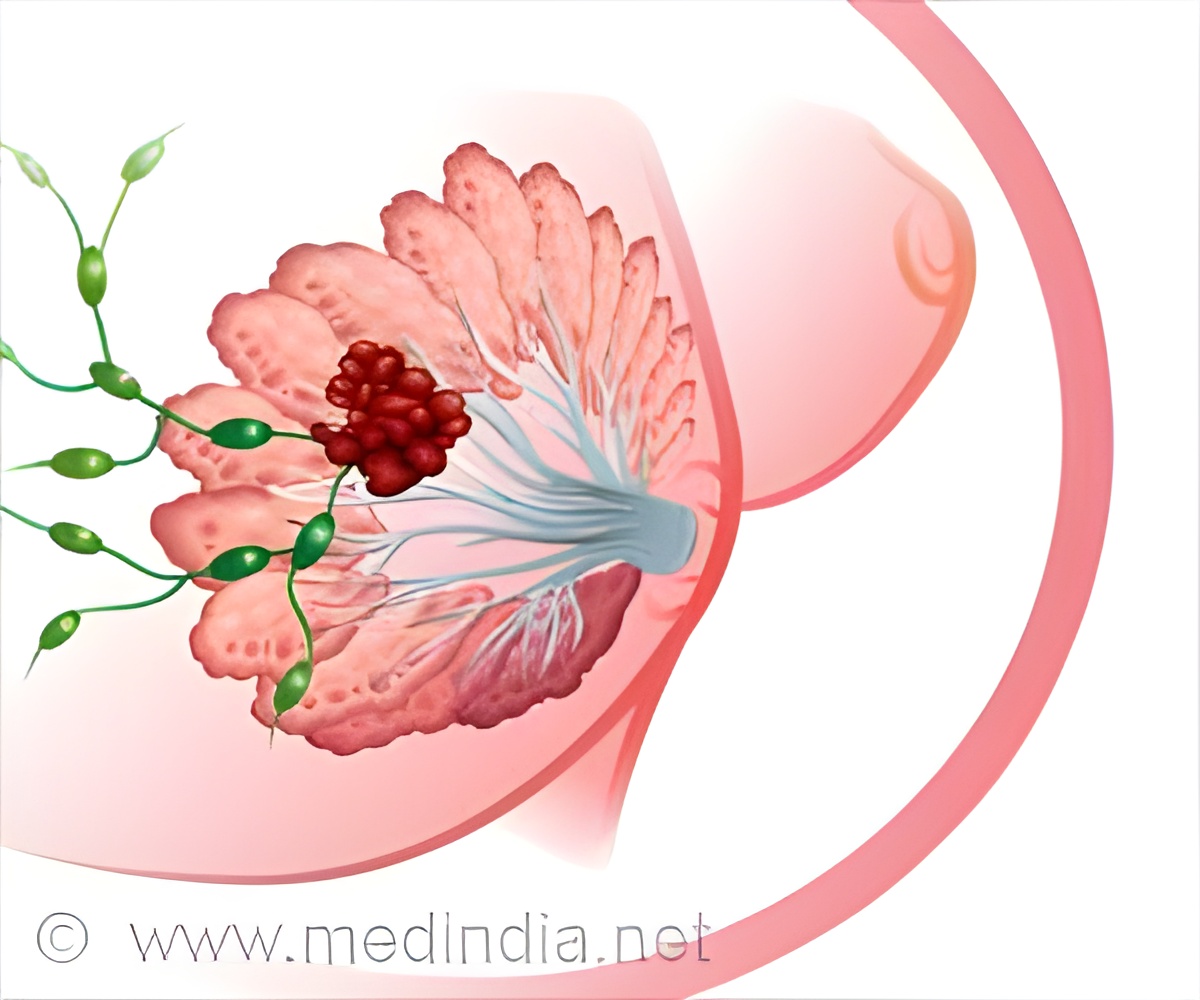
Neoadjuvant systemic therapy (NST) can shrink tumors in breast cancer patients and in some cases allow for breast conserving therapy (lumpectomy) who would otherwise require a mastectomy.
Previous studies have found that lumpectomy with clear margins (no cancer cells in the surrounding tissue) followed by radiation is as effective as mastectomy with no difference in survival. Mastectomies require more extensive surgery and post-surgical recovery. However, women who have undergone a lumpectomy have a slightly higher risk of developing local recurrence of breast cancer.
Golshan and colleagues conducted their analysis as part of BrighTNess, a multi-centered, phase III, double blind, randomized controlled trial sponsored by AbbVie Pharmaceuticals. The trial enrolled 600 women with operable, clinical stage II and III triple-negative breast cancer from 145 centers in 15 countries. Study participants were randomized to receive 12 weeks of one of three different chemotherapy treatment regimens prior to surgery. Before treatment, 458 patients (76 percent) were considered eligible for breast conserving therapy and 141 (24 percent) were deemed ineligible. After treatment, 75 (53 percent) of the patients deemed ineligible were converted to eligible for breast conserving therapy.
Many women who were eligible for a lumpectomy -- including 26 percent of those who tested negative for a genetic mutation for breast cancer -- still underwent a mastectomy. Overall, 342 women (68 percent) who were eligible for breast conserving therapy underwent a lumpectomy. But this rate varied significantly based on where the patient received treatment.
The authors suggest that it may be that higher out-of-pocket costs of mastectomies for patients in Europe or Asia contribute to their findings. In Europe and Asia, removal of the unaffected breast and breast reconstruction are often not covered by insurance unless the patient has a genetic mutation that puts them at risk. In the U.S., such procedures are more frequently covered. The authors note that one of the limitations of their study is that they were unable to ask patients why they made the surgical decision they did and whether insurance coverage influenced their decision.
Source-Eurekalert
 MEDINDIA
MEDINDIA




 Email
Email








