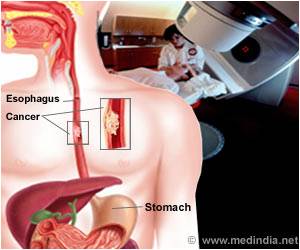
Combining radiotherapy with drugs that rev up a healthy immune response - will help make radiation therapy much more effective.

TOP INSIGHT
Researchers have discover a key mechanism by which immune cells resist radiotherapy and become resistant to further treatment. They have suggested that combining radiotherapy with drugs that rev up a healthy immune response could help make radiation therapy much more effective.
This study was conducted using mouse models of melanoma and focused on the skin where these Langerhans cells are located. However, the researchers believe the same process happens in organs throughout the body. There, cousins of Langerhans cells called dendritic cells are also activated by radiotherapy and the investigators stressed that it is critical we understand how they respond to treatment as well.
Co-author Miriam Merad, Professor of Tumor Immunology, Oncological Sciences, and Hematology and Medical Oncology at The Tisch Cancer Institute at the Icahn School of Medicine at Mount Sinai, said, "Similarly, checkpoint-inhibiting drugs have revolutionized the treatment of melanoma and are being investigated in many other cancers. Cancer has the ability to turn off and even evade the body’s natural immune response to tumors - the new immunotherapy drugs take the brakes off the immune system, promoting a powerful and complete immune response to the cancer."
Dr. Price said, "This is synergized by the addition of radiation, which can expose the tumor so it can better be targeted by the immune system. By combining these treatments, the ability of Langerhans cells to use the immune system to protect cancers will be overwhelmed." Ionizing radiation is a powerful therapeutic tool that causes toxic breaks in cellular DNA. The formation of these breaks triggers a response in Langerhans cells (which are usually dormant) to stop further damage and to repair the breaks.
The researchers discovered that when the skin is damaged by ionizing radiation, Langerhans cells travel to nearby lymph nodes to communicate with other immune cells and help program a population of ’regulatory’ T cells that dampen the immune system. These regulatory T cells then travel back to the damaged tumor, and shield it from attack by the immune system. Dr. Price said, "We found melanoma grew much more quickly on mice pretreated with radiation, compared to untreated mice, because of the presence of regulatory T cells activated by Langerhans cells. These Langerhans cells were resistant to radiation."
Dr. Price further added, "Any treatment that prevents tumor infiltrating regulatory T cells from being produced, such as immunotherapy, will improve the outcome from radiation treatment - and that will save lives."
 MEDINDIA
MEDINDIA



 Email
Email