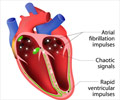
Therapies combining anticoagulant drug with anti-platelet therapy (DAPT) were more effective in preventing bleeding complications in atrial fibrillation.

TOP INSIGHT
Therapies combining the anticoagulant drug rivaroxaban with either single or dual anti-platelet therapy (DAPT) were more effective in preventing bleeding complications in atrial fibrillation.
Principal Investigator C. Michael Gibson, Chief of Clinical Research in the Division of Cardiovascular Medicine at BIDMC, reported the new research findings online in The New England Journal of Medicine and simultaneously presented the findings at the American Heart Association's Scientific Sessions 2016 in New Orleans.
The PIONEER AF-PCI randomized clinical trial involved more than 2,100 patients at 430 sites in 26 countries.
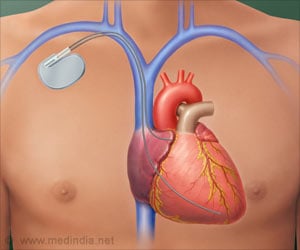
"In managing the stented patient with atrial fibrillation, a pharmacologic strategy must carefully balance the risk of stent thrombosis, or blood clot, with the risk of bleeding complications," said Gibson, who is also Professor of Medicine at Harvard Medical School and chairman of the PERFUSE (Percutaneous/Pharmacologic Endoluminal Revascularization for Unstable Syndromes Evaluation) Study Group. "This trial, which tested two entirely new strategies, now provides us with randomized clinical trial data demonstrating that a combination of rivaroxaban with anti-platelet therapy is successful in minimizing bleeding while preventing clotting."
Current guidelines call for combining three drugs - DAPT plus a vitamin K antagonist (VKA) anticoagulant - in a strategy known as "triple therapy." But as the authors note, this approach may result in excess major bleeding rates of 4 to 12 percent within the first year of treatment.
The findings showed that among patients with atrial fibrillation who underwent intracoronary stent placement, the administration of rivaroxaban in one of two dose strategies reduced the risk of clinically significant bleeding in about one out of every 10 to 11 patients as compared with triple therapy including a vitamin K antagonist. The risks of rehospitalization and death from all causes were also reduced in about one out of every 10 to 15 cases.
Source-Eurekalert
 MEDINDIA
MEDINDIA

 Email
Email