Ovarian cancers metastasize through a distinct mechanism that results in several lesions anchored throughout the abdominal cavity, making surgery challenging.
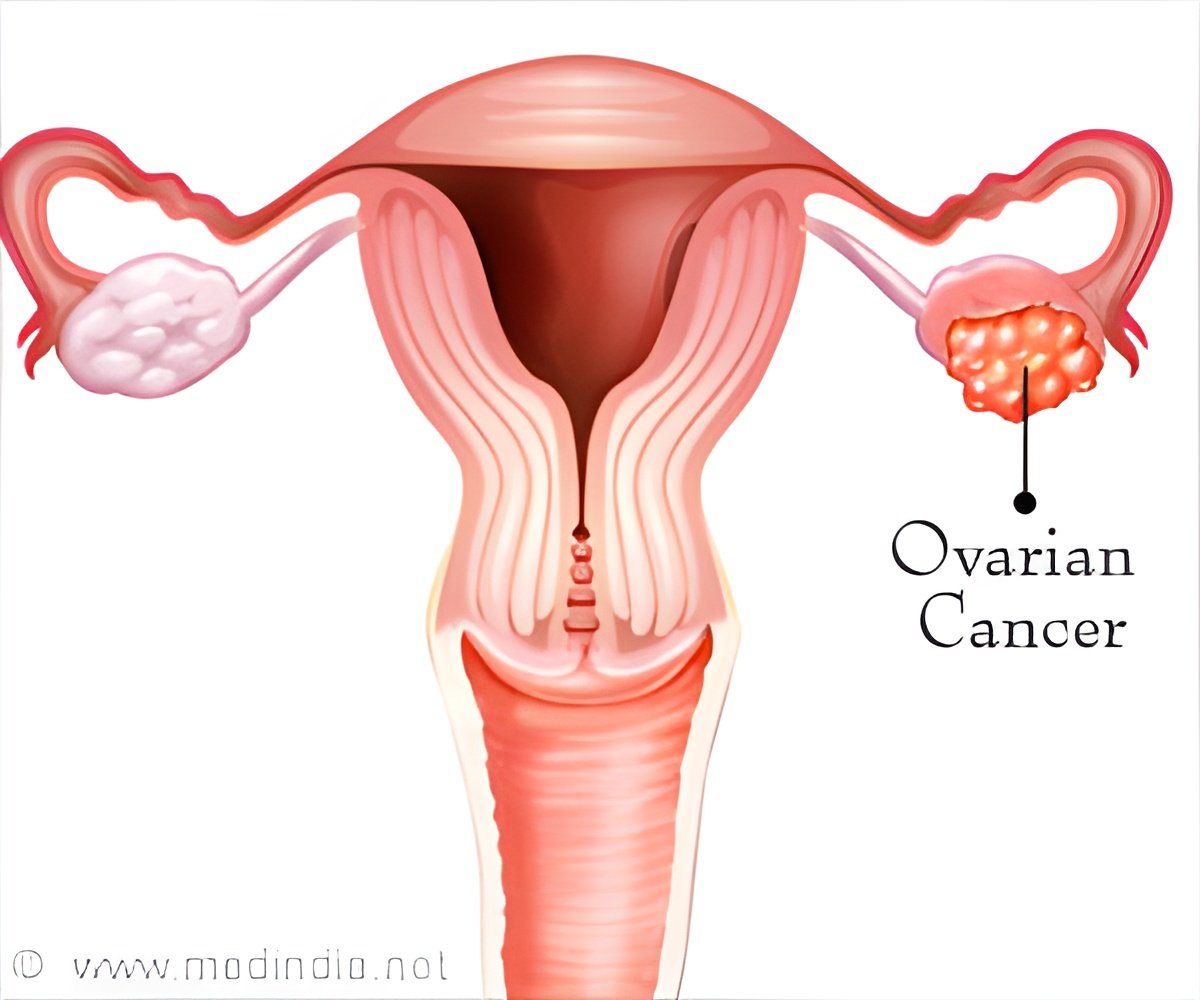
‘An increased BMI is associated with a greater risk for ovarian cancer with worse overall survival. Ovarian cancers metastasize through a distinct mechanism that results in large numbers of lesions anchored throughout the abdominal cavity, making surgery challenging.’





M. Sharon Stack, Ann F. Dunne and Elizabeth Riley Director of the HCRI and professor of chemistry and biochemistry, notes that ovarian cancer is the leading cause of death from gynecologic malignancy in the US. The researchers set out to determine whether obesity contributes to ovarian cancer metastatic success. In other words, are tumor cells better able to successfully metastasize when the 'host' is obese versus lean? Stack said, "Ovarian cancers metastasize through a distinct mechanism that results in large numbers of lesions anchored throughout the abdominal cavity, making surgery challenging."
Stack and Harper researcher Yueying Liu led a team of researchers that used an integrative approach combining three-dimensional cell culture models, tissue explants and mouse models to evaluate tumor cell adhesion to the cells which line the abdominal cavity, called mesothelial cells.
Stack said, "In 3-D tissue culture models, we found that lipid-loading the mesothelial cells, or growing them in the presence of components that make up fat, increased the ability of tumor cells to bind to them. As tumor cell-mesothelial cell binding is a key step in ovarian cancer metastasis, this prompted us to study this further in mouse models. We used a 'diet-induced obesity' (DIO) protocol in which mice were fed a high fat diet, which was 40% fat, relative to mice fed control chow. When mice were significantly different in weight, they were injected with fluorescent ovarian cancer cells and we monitored metastatic seeding in the abdominal cavity by in vivo imaging."
Individual organs were removed from the mice and imaged to quantify tumor burden in each organ. Researchers also used another mouse model of obesity termed the ob/ob mouse which harbored a mutation that caused it to become highly obese.
Advertisement
Stack further added, "Our ongoing efforts are aimed at understanding the mechanism by which obesity impacts metastatic success. For example, we have found that tumors growing in obese host mice turn on lipid synthesis and lipid transport, suggesting that they are better able to acquire and utilize nutrients from fat. The blood supply to the tumors is also impacted, as is the presence of specific immune cells. There is still a lot of work needed to figure out where we can intervene in this process."
Advertisement
Stack also noted that the interdisciplinary nature of the research. She said, "In addition to the cell-based research, we analyzed hundreds of fluorescent images and many hundreds of slides to collect the data to support our conclusions. We had phenomenal interactions with the Harper Tissue Biorepository and the Notre Dame Integrated Imaging Facility. You can see the team effort by looking at the author listing: This paper has 22 authors! Seven of them are current or former ND undergrads and four are current or former ND grad students."
The study appears in Cancer Research.
Source-Eurekalert