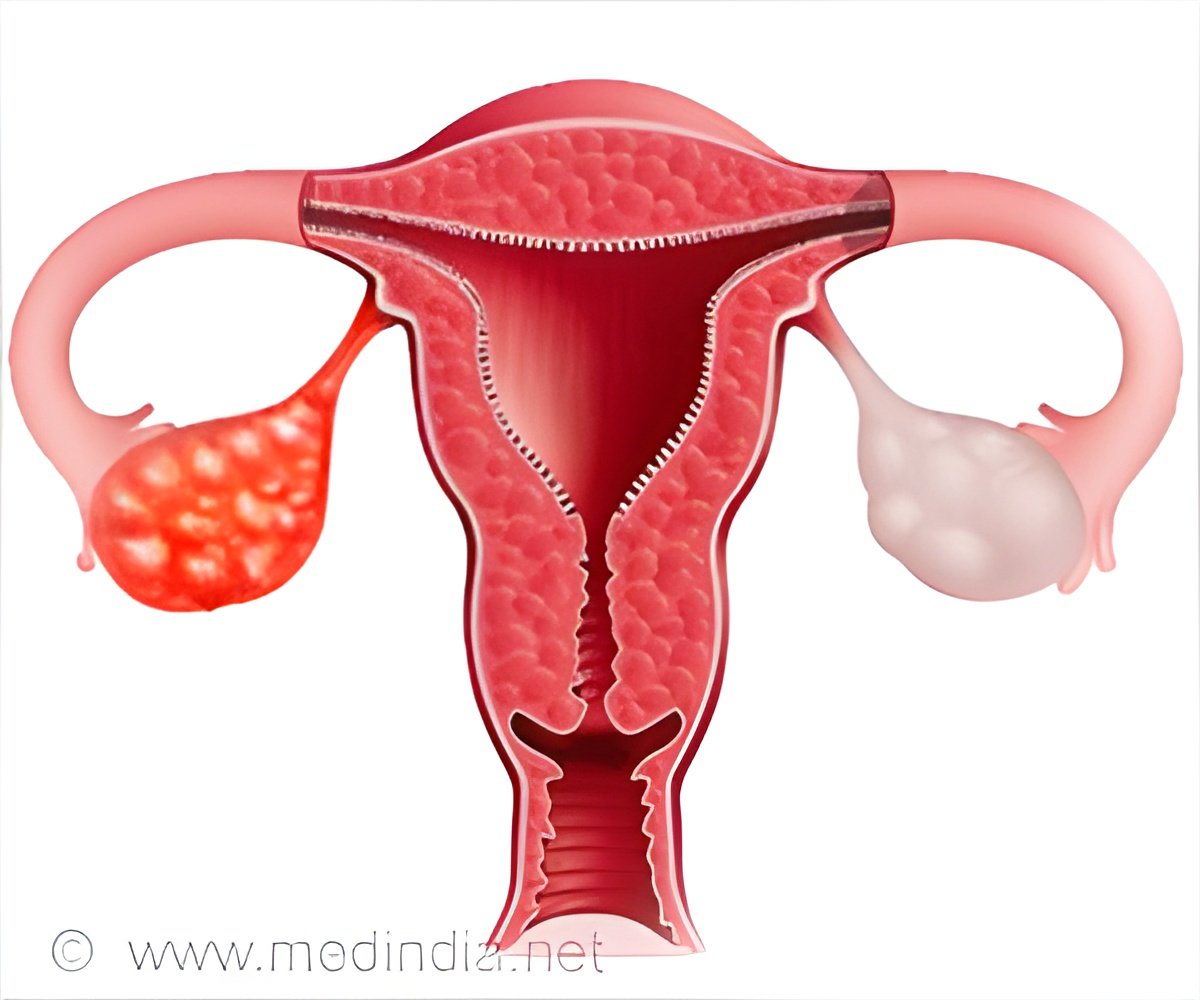
Researchers were able to identify several lncRNAs that are linked to the disease,by evaluating the molecular changes that occur in large cohorts of ovarian cancer patients.
‘EMT is important for cell migration and invasion - two characteristics of metastatic cancer cells -- strongly suggesting that the link between lncRNAs and EMT contributes to the metastatic progression of ovarian cancer.’





The research, which appears in a recent issue of Nature Communications, was spearheaded by lead author and bioinformatician Dr. Ramkrishna Mitra, a postdoctoral associate in the Eischen laboratory. Dr. Mitra undertook a large-scale bioinformatics approach to evaluate over 700 ovarian cancer molecular profiles from four patient cohorts. This analysis led to the identification of several lncRNAs that are overexpressed in a particular subset of ovarian cancer, those that are thought to be the most aggressive.Further analysis revealed that overexpression of these lncRNAs in turn changed the expression of proteins that regulate a well-known developmental process, termed the epithelial-to-mesenchymal transition (EMT).
Following up on this idea, the researchers found that one of the lncRNAs was directly implicated in patient outcomes. "Overexpression of one of the lncRNAs, DNM30S, was significantly correlated with worse overall ovarian cancer patient survival," said Dr. Eischen.
Based on these observations, the researchers suggest that targeting of the lncRNAs might represent a viable treatment strategy for ovarian cancer. To test this idea, they experimentally reduced the expression of the DNM30S lncRNA, which resulted in reduced ovarian cancer cell migration and invasion. In future work, the Eischen laboratory aims to further understand the role of lncRNAs in ovarian cancer, and potentially translate their findings into clinical applications to reduce ovarian cancer metastasis.
Advertisement



![Prostate Specific Antigen [PSA] & Prostate Cancer Diagnosis Prostate Specific Antigen [PSA] & Prostate Cancer Diagnosis](https://images.medindia.net/patientinfo/120_100/prostate-specific-antigen.jpg)