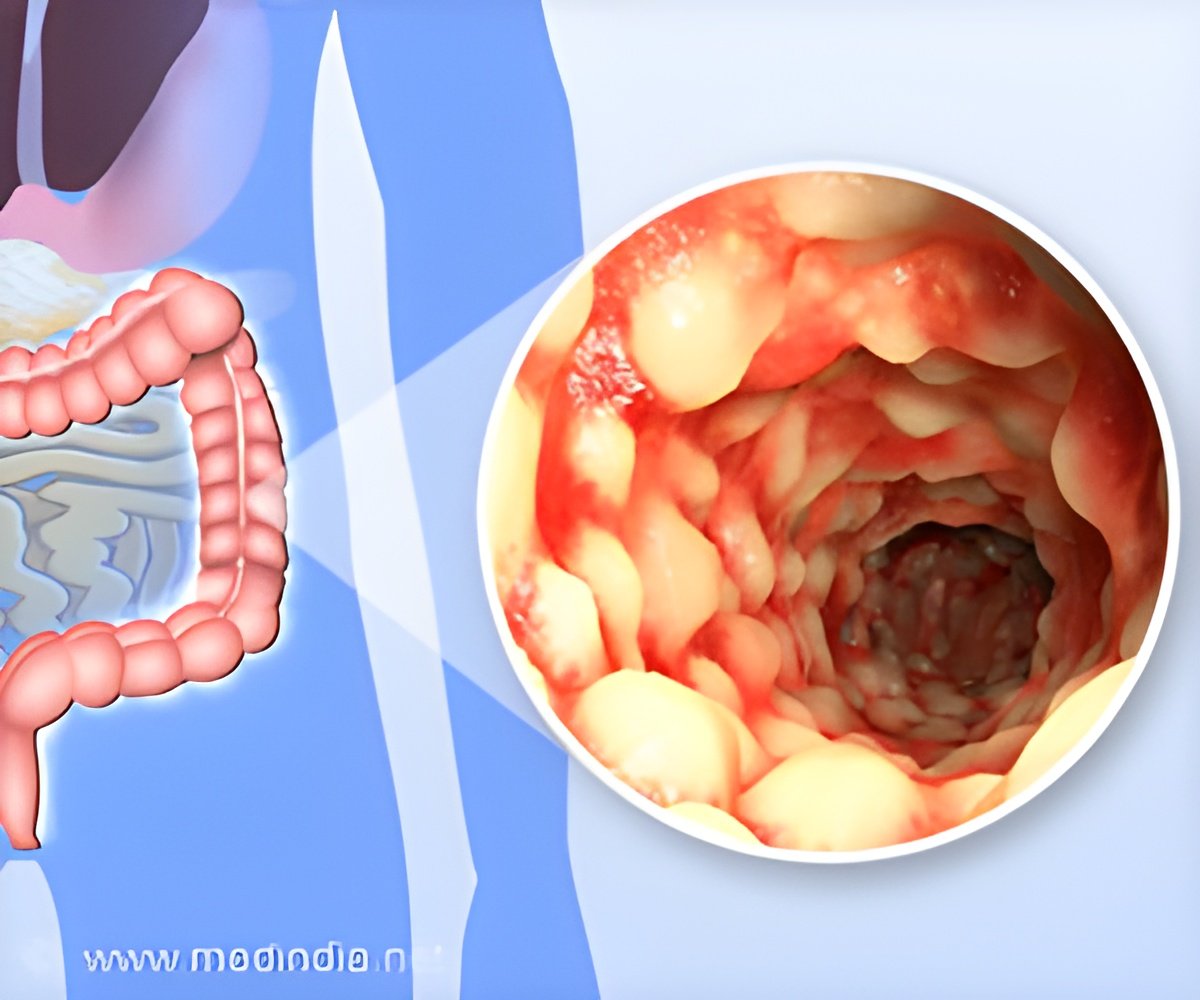
For individuals with inflammatory bowel disease (IBD), the routine act of eating and nutrient absorption can vary significantly.
Doctors Discover Many Patients at UNC’s Inflammatory Bowel Disease Clinic Screen Positive for Malnutrition
Go to source).
TOP INSIGHT
In the realm of inflammatory bowel disease (IBD), the commonplace act of eating takes on a different dimension, with chronic inflammation of the digestive tract causing malnutrition. The pressing revelation of high malnutrition rates among IBD clinic patients underscores the vital necessity for same-day dietitian support, given the elevated risks of morbidity and mortality. #inflammatoryboweldisease, #malnutrition, #crohn'sdisease, #ulcerativecolitis
Between June 7, 2022, and July 19, 2022, 237 IBD patients were screened. Results showed that 14% of those patients were at high risk for malnutrition.
The prevalence of a positive screen was 15% among patients with Crohn’s disease and 12% among patients with ulcerative colitis.
“It was important to do this study because we have limited time with our patients and often many problems to address,” said Anne F. Peery, MD, corresponding author and associate professor of medicine at the UNC School of Medicine.
“It’s easy to miss malnutrition in the clinic setting.”
If yes, how much weight have you lost? Have you been eating poorly because of a decreased appetite? One key factor to highlight was that most patients in the cohort had a normal or overweight body mass index, showing that malnutrition risk can develop at any body weight.
Impact of IBD on Digestive Health
Symptoms such as diarrhea, abdominal pain, fever, nausea, low energy, and loss of appetite are all signs of active disease. The study showed that 28% of the patients in an IBD flare met the criteria for malnutrition.“A positive screen for malnutrition should be immediately followed up with a formal nutrition assessment,” said Peery, who is also director of the Adult Inpatient Nutrition Support Team in the Division of Gastroenterology and Hepatology at the Department of Medicine.
“A registered dietitian in the clinic can fill this gap in care and can help the team develop a plan to meet the patient’s nutrition needs. We are fortunate to now have a full-time registered dietitian with us in the GI clinic. She has significantly improved the care we provide.”
“Moving forward, it would be useful to have our care partners in the clinic who room the patient and also screen the patients for malnutrition,” said Peery.
This study is another example of how patients with IBD do best when they receive multidisciplinary care.
A registered dietitian can help the team identify any deficiencies, estimate the patient’s energy and protein needs, and help develop a plan to meet these needs. This study was funded in part by the National Institutes of Health.
Reference:
- Doctors Discover Many Patients at UNC’s Inflammatory Bowel Disease Clinic Screen Positive for Malnutrition - (https://news.unchealthcare.org/2023/12/doctors-discover-many-patients-at-uncs-inflammatory-bowel-disease-clinic-screen-positive-for-malnutrition/)
Source-Eurekalert
 MEDINDIA
MEDINDIA




 Email
Email