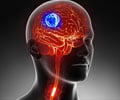
Surgically treated brain for glioblastoma might acquire enhanced CAR-T immunotherapy benefits by incorporating a newly developed gel with the therapy.
Surgically treated brain for glioblastoma might acquire enhanced CAR-T immunotherapy benefits by incorporating a newly developed gel with the therapy as per a study
“Fibrin gel enhances the antitumor effects of chimeric antigen receptor T cells in glioblastoma”, at the University of North Carolina Lineberger Comprehensive Cancer Center, published in the journal
Science Advances.
Glioblastoma is a highly malignant and deadly brain cancer arising from glial cells (brain cells for supporting and nourishing neurons). It is diagnosed commonly at the age of 60s in people. It is estimated that only 40% of people live for one year after diagnosis and 17% for two years.
TOP INSIGHT
Surgically treated brain for glioblastoma might acquire enhanced CAR-T immunotherapy benefits by incorporating a newly developed gel with the therapy.
from a patient and genetically re-engineering them in the lab to recognize targets on the surface of cancer cells.
New Gel and Immunotherapy
The team used CAR-T cell immunotherapy in the mouse model with surgically removed glioblastoma. Earlier studies revealed no greater benefits from the administration of T cells. However, the present study showed that
incorporating gel with immunotherapy enhanced the benefits of immunotherapy.
“We developed a gel made of fibrin, a protein most often associated with helping blood to clot. Applying a gel substance to an area of the brain to aid CAR-T cell therapy is unique in glioblastoma treatment. The gel aided CAR-T cell distribution in the brain by acclimating the T cells to the post-surgical wound environment while also stopping the tumor from recurring,” says Edikan Ogunnaike, Ph.D., a biomedical engineer at UNC and first author of the article.
The study showed that
9 out of 14 (64%) mice that received the gel and T cells were tumor-free 94 days after treatment, compared to two of 10 (20%) mice who only received T cells.
“Our approach was beneficial in glioblastoma and we believe that it could also control growth or return of tumors in the brain, eye and other organs. It should be noted that direct delivery of CAR-T cells into a post-surgical area must result in broad coverage of the surface of the surgical cavity to maximize the possibility that T cells come in contact with residual tumor cells, which is where our flexible scaffold has shown to be of great benefit,” says Gianpietro Dotti, MD, professor in the UNC School of Medicine Department of Microbiology and Immunology, co-leader of the Immunology Program at UNC Lineberger and corresponding author of this article.
Source-Medindia
 MEDINDIA
MEDINDIA


 Email
Email