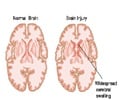
When the optic nerve is injured, there are tears and swelling in the affected area that causes the nerve cells to die causing vision loss.

- Head injury sometimes results in irreversible loss of vision.
- The optic nerve that is responsible for passing information between the eyes and the brain is damaged.
- Nerve cells in the brain die in response to the injury in the optic nerve. This type of injury is called traumatic optic neuropathy.
TOP INSIGHT
Inflammation brought on by white blood cells play a role in head trauma-induced vision loss. Limiting inflammation could decrease nerve damage and preserve cell function.
Wenbo Zhang, UTMB associate professor in the department of ophthalmology & visual sciences, and his team found that inflammation brought on by white blood cells play a role in head trauma-induced vision loss. Limiting inflammation could decrease nerve damage and preserve cell function, researchers discovered.
Inflammation is part of the body's defense system against injury and infection and is an important component of wound healing. White blood cells travel to injured areas to help repair the damaged tissue, causing inflammation in the process.
Excessive or uncontrolled inflammation can actually make injuries worse and contribute to disease in a couple of different ways - by activating cell death processes, clogging and rupturing blood vessels and producing toxic molecules like free radicals.
"Our data clearly showed that one of the protein receptors on white blood cells called CXCR3 brings white blood cells to the optic nerve in response to production of its binding partner CXCL10 by damaged nerve tissue," said Zhang.
Yonju Ha, a lead author of this article, said that further studies on this receptor and its role in white blood cell recruitment following tissue injury may aid in the development of new interventions for diseases associated with nerve injury, such as TON, stroke, diabetic retinopathy and glaucoma.
- Wenbo Zhang et al., UTMB researchers discover reason for permanent vision loss after head injury, American Journal of Pathology (2017) .
Source-Medindia
 MEDINDIA
MEDINDIA



 Email
Email