An immune-boosting compound increases the efficacy of immunotherapy against pancreatic cancer. The new drug promotes the killing of the cancer cells, resulting in the reduction of tumor size and longer life span.
- A new immune-boosting drug molecule has been discovered
- The drug boosts the effectiveness of immunotherapy against pancreatic cancer
- This leads to a reduction in tumor size and prolongation of life
The results, published in Science Translational Medicine, suggest that the new drug molecule could make resistant pancreatic cancer cells responsive to immunotherapy, which will help enormously to fight the disease.
The study was jointly led by Dr. David G. DeNardo, PhD and Dr. Vineet Gupta, PhD. Dr. DeNardo is an Associate Professor in the Departments of Medicine, Pathology, and Immunology at the Washington University School of Medicine in St. Louis, Missouri, USA. Dr. Gupta is the Vice-Chair for Research and Innovation in the Department of Internal Medicine and Director of the Drug Discovery Center at Rush University, Chicago, Illinois, USA.
The first author of the paper was Dr. Roheena Panni, MD, MPHS, who is a Resident in General Surgery in the Department of Surgery, Washington University School of Medicine in St. Louis, USA.
The co-author of the paper was Dr. William Hawkins, MD, who is the Neidorff Family and Robert C. Packman Professor of Surgery and Chief, Section of Hepatobiliary-Pancreatic and Gastrointestinal Surgery, Washington University School of Medicine in St. Louis, USA.
Read More..
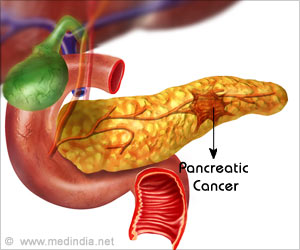
Pancreatic Cancer: Facts & Figures
- Pancreatic cancer is the third leading cause of cancer deaths in the US
- Treating pancreatic cancer is a major challenge
- Chemotherapy, radiation therapy, and immunotherapy are by and large ineffective against pancreatic cancer
- 8 percent of patients live more than 5 years post-diagnosis
- 3 percent of clinical trials on cancer immunotherapy target pancreatic cancer
What are the Challenges of Immunotherapy against Pancreatic Cancer?
Harnessing the power of the immune system is a major challenge of immunotherapy against pancreatic cancer. Immunotherapy against pancreatic cancer is based on disinhibition of immune T-cells so that they attack the cancer cells. Although this technique has been successful in the lab, it hasn’t worked in actual pancreatic cancer patients, where improvement was noted in fewer than 5 percent of cases. These poor results discouraged the clinical use of immunotherapy for pancreatic cancer.Instead of T-cells, the researchers focused on another class of immune cells, called myeloid cells, which have the capability of stimulating, as well as inhibiting the immune response. In the case of pancreatic cancer, these myeloid cells have been found to inhibit the immune response against the cancer cells, thereby reducing the efficacy of immunotherapy.
The research team realized that disinhibition of T-cells wouldn’t be enough to kill the pancreatic cancer cells. They felt sure that boosting immunotherapy would also require the mobilization of those classes of myeloid cells, which would stimulate T-cells to attack the cancer cells.
How Did the Researchers Overcome the Challenges?
The researchers eventually overcame the challenges associated with boosting the efficacy of immunotherapy. They discovered a new drug molecule called ADH-503 (a CD11b agonist), which alters the migration of myeloid cells in the body. Normally, myeloid cells are plentiful in the vicinity of pancreatic tumors, where they suppress the immune attack against the tumors.When administered in mice with pancreatic cancer, ADH-503 significantly reduced the number of myeloid cells surrounding the tumors. The only myeloid cells that were left were those that stimulated T-cells to attack the pancreatic tumors. This led to a rise in the cancer-killing T-cell population, reduction in tumor size, and longer survival of mice.
The research team also investigated whether creating a similar milieu would increase the susceptibility of pancreatic tumors to standard immunotherapy. To test this hypothesis, they injected mice with PD-1 (programmed cell death protein 1), which is used in standard immunotherapy against several cancers. But there was no response. However, when PD-1 was administered along with ADH-503, the tumors dramatically reduced in size and the mice survived for over 4 months, whereas all the control mice died within 6 weeks. In some cases, the tumors resolved completely, thereby curing the mice of pancreatic cancer.
“Pancreatic cancer is a highly lethal disease, and we are in desperate need of new therapeutic approaches,” says DeNardo. He adds: “In animal studies, this small molecule led to very marked improvements and was even curative in some cases. We are hopeful that this approach could help pancreatic cancer patients.”
Future Plans
The research team plans to test the new drug molecule in humans and are planning Phase I clinical trials later on this year.In this regard, DeNardo says: “You can’t make a one-to-one translation between animal studies and people, but this is very encouraging.” He adds: “More studies are needed to understand if the compound is safe and effective in people, which is why this compound is going into Phase I safety studies in people later this year at Washington University and other sites.”
Concluding Remarks
Boosting the immune response by modulating the myeloid cells improves the effectiveness of other therapies against pancreatic cancer too. For example, mice treated with ADH-503, respond much better to both chemotherapy and radiotherapy.Gupta concludes: “Unlocking the promise of immunotherapies for pancreatic cancer requires a new approach.” He adds: “We believe these data demonstrate that targeting myeloid cells can help overcome resistance to immunotherapies.”
Funding Source
The study was funded by the National Institutes of Health, the NIH/National Cancer Institute, the Department of Defense, and the National Center for Research Resources, USA.Reference:
- Agonism of CD11b Reprograms Innate Immunity to Sensitize Pancreatic Cancer to Immunotherapies - (https://stm.sciencemag.org/content/11/499/eaau9240.full)
Source-Medindia