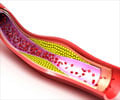
The experimental drug doubles the levels of good cholesterol and lowers bad cholesterol and yet has no effect on cardiac events.

TOP INSIGHT
Evacetrapib, an experimental drug shows potential to raise levels of HDL or good cholesterol in the arteries but fails to improve overall heart health.
The study involving more than 12,000 patients at high risk for serious cardiovascular problems found that evacetrapib had no benefits, according to research presented at the American College of Cardiology conference in Chicago.
Manufacturer Eli Lilly stopped the trial in October when the drug was found to be ineffective but now experts have given a comprehensive explanation of what happened.
Two other drugs in the same class as evacetrapib, known as CETP inhibitors and designed to raise levels of HDL cholesterol -- high-density lipoprotein, the "good" type -- have also failed, presenting experts with a quandary.
"We have a paradox: here we've got an agent that more than doubles the levels of good cholesterol and lowers bad cholesterol and yet has no effect on clinical events," said lead author Professor Stephen Nicholls.
On average, patients taking evacetrapib daily for at least 18 months lowered their LDL cholesterol by 37 percent and increased their HDL cholesterol -- high-density lipoprotein, the "good" type -- by 130 percent compared with patients taking a placebo.
"As we close out the trial, we're trying to understand how a drug that seems to do all the right things in terms of blood cholesterol levels doesn't then translate into reducing clinical events," added Nicholls.
Steve Nissen, chairman of Cardiovascular Medicine at Cleveland Clinic, attempted to put a positive spin on the disappointing outcome.
"These findings illustrate the importance of performing large, high-quality outcome trials," he said.
"Just looking at the effects a therapy has on cholesterol levels doesn't always translate into clinical benefits."
However, Nicholls cautioned that evacetrapib could potentially benefit patients with low risk of serious heart trouble, although that was not part of the study.
The findings could challenge conventional thinking regarding the benefits of HDL cholesterol in protecting against cardiovascular problems, he said.
They also suggest that existing treatments, such as statins, are already so effective that they cannot be improved upon.
However, some people with high cholesterol were hoping for an alternative to statins because they complain about side effects such as muscle pain and weakness.
Source-AFP
 MEDINDIA
MEDINDIA



 Email
Email