The source of damaging inflammation after a heart attack has been identified by experts who also claimed that there is an already approved drug which can effectively tamp down such inflammation and protects the heart from progressive damage after a heart attack.

TOP INSIGHT
The source of inflammation in the heart after a heart attack has been identified by experts who also suggested that a drug called ‘pirfenidone’ may reduce this type of inflammation.
Led by senior author Douglas L. Mann, MD, director of the university’s Cardiovascular Division and cardiologist-in-chief at Barnes-Jewish Hospital, the study showed that mice modeling human heart attacks lived longer if then given pirfenidone, a drug already approved to treat an unrelated lung condition. Further, the research showed that the drug works by regulating in the heart the specific response of B cell lymphocytes, the immune cells that the scientists discovered were responsible for the inflammation.
"If we understand how pirfenidone works to reduce inflammation, we can work to modify the drug or make an even better drug that may be able to help a large number of patients," said Mann, who is also the Tobias and Hortense Lewin Distinguished Professor of Cardiovascular Diseases.
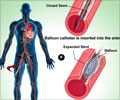
In a heart attack, blood is cut off from an area of the heart that then often dies. If the person survives, the body tries to heal the dead muscle by forming scar tissue -- but such tissue can further weaken the heart. Yet another wave of damage can occur when well-intentioned immune cells try to heal the injured heart but instead drive inflammation. Finding ways to prevent progressive inflammatory injury to the heart could help some 1.5 million heart attack patients in the U.S. annually, potentially preventing their progression to heart failure, according to the researchers.
Pirfenidone is approved by the Food and Drug Administration to treat a lung condition called idiopathic pulmonary fibrosis, a scarring of the lungs that has no known cause. The drug also has been known for its heart-protective effects in a number of different animal models of heart attack. Researchers had assumed that pirfenidone’s protective action in the heart paralleled the reason it helps in lung disease. In the lungs, the drug slows the formation of scar tissue.
Adamo said that most immune studies of the heart have focused on other types of immune cells, including macrophages, T cell lymphocytes, neutrophils and monocytes. But he found no differences in the numbers of such immune cells in the injured hearts of mice that received pirfenidone versus those that didn’t. When he serendipitously measured B cells, however, Adamo was surprised to see a huge difference.
However, Adamo added that when the researchers removed these cells completely, not only was the heart not protected, the beneficial effect of the drug went away. So the B cells are not exclusively bad, according to the scientists. If they were, removing them completely would protect the heart. "The protective effects of pirfenidone hinge on the presence of B cells," Adamo said. "The drug may be working on other cells as well, perhaps directly or perhaps through the B cells. We’re continuing to investigate the details."
Adamo said that pirfenidone has long been considered safe but that it can have side effects such as nausea and vomiting. He explained that researchers have not tried to improve upon the drug because no one understood precisely how it worked. Now that Adamo, Mann and their colleagues have identified B cell lymphocytes as the drug’s target, they can begin investigating ways to make it better. With the support of Washington University’s Office of Technology Management, the scientists have launched a startup company focused on designing a version of pirfenidone that maintains the drug’s ability to modulate B cell lymphocytes but that may be more tolerable for patients.
The study is published in JCI Insight.
Source-Eurekalert
 MEDINDIA
MEDINDIA




 Email
Email