A migraine history should be considered a significant risk factor for pregnancy complications like premature birth, gestational hypertension, and pre-eclampsia.
- Migraine affects women disproportionately, especially throughout their reproductive years
- Pre-pregnancy migraine increased the chance of problems such as premature birth, gestational hypertension, and pre-eclampsia
- This suggests that migraine can be a clinical marker of elevated obstetric risk
TOP INSIGHT
Pregnancy migraine was associated with a 17% increased risk of preterm delivery, a 28% increased risk of gestational hypertension, and a 40% increased risk of pre-eclampsia as compared to no migraine.
Link between Migraine and Pregnancy Problems
The Brigham researchers reviewed data from hundreds of women in the Nurses' Health Study II to determine the link between migraines and pregnancy problems. Their findings suggest that a history of migraines may be an indicator of increased obstetric risk.“Preterm delivery and hypertensive disorders are some of the primary drivers of maternal and infant morbidity and mortality,” said Alexandra Purdue-Smithe, associate epidemiologist at Brigham and instructor in Medicine at Harvard Medical School. “Our findings suggest that a history of migraine warrants consideration as an important risk factor for these complications and could be useful in flagging women who may benefit from enhanced monitoring during pregnancy,” Purdue-Smithe added.
Women Have a Higher Risk of Migraines
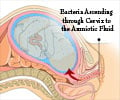
Women are two to three times more likely than males to suffer from migraines throughout their lifetime, and headaches are most common between the ages of 18 and 44 when women are most fertile.Aura (5.5% of the population) can accompany migraine headaches, which are typically visual abnormalities that develop before headache onset.
The researchers evaluated data from the Nurses' Health Study II, which comprised 30,555 pregnancies from 19,694 U.S. nurses, for this study. The researchers examined pre-pregnancy self-reported physician-diagnosed migraine and migraine phenotype (migraine with and without aura), as well as the incidence of self-reported pregnancy outcomes.
Pre-pregnancy migraine was found to be connected with a 17% higher risk of preterm delivery, a 28% higher rate of gestational hypertension, and a 40% higher rate of preeclampsia compared to no migraine.
Migraine with aura was linked to an increased incidence of preeclampsia compared to migraine without aura.
Aspirin Use Linked with Preterm Delivery
Participants with migraines who reported regular aspirin use — more than twice weekly — before pregnancy had a 45% decreased risk for preterm delivery. Individuals at high risk of preeclampsia and those with more than one intermediate risk factor for preeclampsia should take low-dose aspirin throughout pregnancy, according to the US Preventive Services Task Force.Low-dose aspirin during pregnancy has also been found in clinical trials to reduce premature birth rates. However, Purdue-Smithe pointed out that migraines are not among the indications for aspirin use during pregnancy.
“Our findings of reduced risk of preterm delivery among women with migraine who reported regular aspirin use before pregnancy suggests that aspirin may also be beneficial for women with migraine,” Purdue-Smithe said. “Given the observational nature of our study, and the lack of detailed information on aspirin dosage available in the cohort, clinical trials will be needed to definitively answer this question.”
Source-Medindia
 MEDINDIA
MEDINDIA





 Email
Email