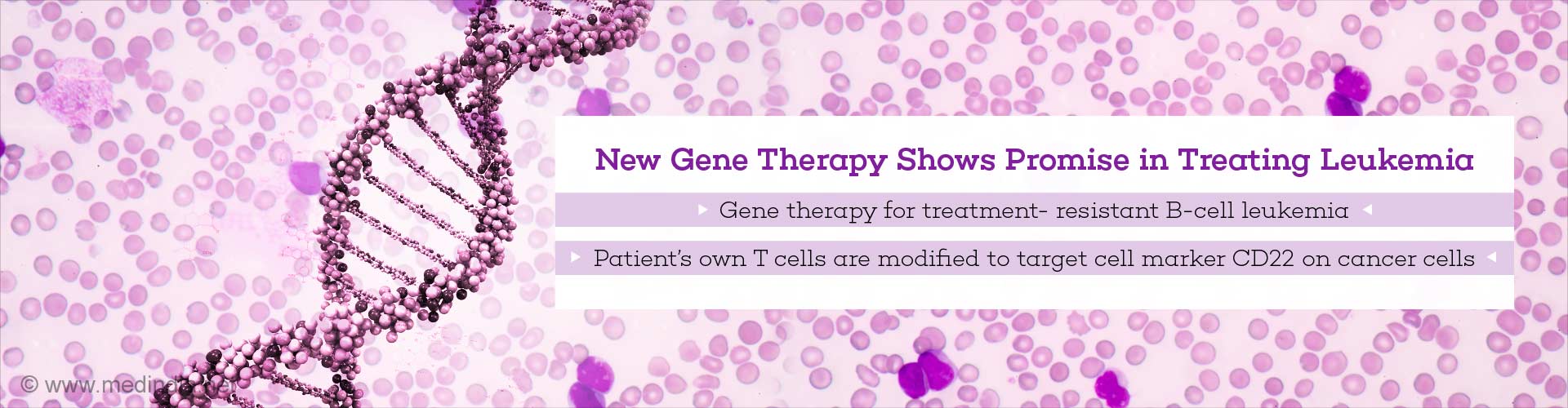
New gene therapy targeting a cell marker shows promise in treating treatment- resistant B-cell leukemia.
TOP INSIGHT
Anti-CD22 CAR T-cell therapy modifies the patient’s T cells by training it to target cancer cells that carry the CD22 cell surface marker.
Highlights:
- New gene therapy shows promise as a therapeutic for treatment- resistant B-cell leukemia.
- The therapy alters the patient’s own immune cells to target a molecular marker called CD22.
- New prospects include a gene therapy approach that targets both the CD19 and CD22 markers.
Treatment- resistant B-cell leukemia
B-cell acute lymphoblastic leukemia is the most common cancer in children and chemotherapy is the standard treatment. However, there are groups of patients who do not respond to chemotherapy. There are also groups of patients who experience a relapse in the cancer after successful remission. This type of B cell leukemia can be characterized as treatment resistant.CAR T-cell therapy
CD19-targeted chimeric antigen receptor T-cell therapy, or CAR T-cell therapy is the original gene therapy that showed promising results for treating treatment- resistant B-cell leukemia. This FDA approved therapy modifies the patients T cells to target the molecular marker CD19 expressed on the surface of cancer cells. However, recent studies have shown that in some patients who undergo CD19-targeted CAR T-cell therapy, their cancer cells stop expressing the CD19 molecule on their cell surfaces. In fact 15 out of 21 patients who were enrolled in the treatment either relapsed or failed to respond to the treatment.Anti-CD19 CAR T-cell therapy: The new gene therapy
This therapy is similar to but distinct from the anti-CD19 CAR T-cell therapy. The primary and key difference is in the molecular marker it targets. The new therapy targets another key molecular marker on the cell surface of cancer cells: CD22. This therapy modifies the patient’s own T cells, a type of immune cells, to kill cancer cells by training them to recognize CD22 marker on the surface."This is the first time that we've seen response rates anything like we achieved when we were first testing the CD19 CAR T therapy," said Crystal Mackall, MD, the associate director of Stanford's Cancer Institute and the director of the Parker Institute for Cancer Immunotherapy at Stanford. "We were all a little worried that we wouldn't find anything comparable. But this study gives hope to the idea that there may be another similar, very potent treatment."
The research team hopes to develop a therapy that targets both the CD19 and CD22 markers—an approach the team believes the cancer cells cannot evade.
The Phase I study
The study enrolled patients aged 7 to 30 with B cell acute lymphoblastic leukemia. The participants received varying doses of the anti-CD22 CAR T-cell therapy and all of them had received at least one bone marrow transplant. Moreover, 10 out of the 15 patients who previously received the CD19 treatment no longer expressed CD9 on their cancer cells.At the lowest dosage 1 out of 6 patients achieved complete remission. At the next higher dosage 11 out of 15 achieved remission. The median remission period was 6 months with 3 patients remaining in complete remission at six, nine and 21 months after the therapy.
"The take-home message is that we've found another CAR T-cell therapy that displays high-level activity in this phase-1 trial," said Mackall. "But the relapse rate was also high. So this forces the field to get even more sophisticated. How much of a target is needed for successful, long-lasting treatment? What happens if we target both CD19 and CD22 simultaneously?"
Reference:
- Terry J Fry, Nirali N Shah, Rimas J Orentas, Maryalice Stetler-Stevenson, Constance M Yuan, Sneha Ramakrishna, Pamela Wolters, Staci Martin, Cindy Delbrook, Bonnie Yates, Haneen Shalabi, Thomas J Fountaine, Jack F Shern, Robbie G Majzner, David F Stroncek, Marianna Sabatino, Yang Feng, Dimiter S Dimitrov, Ling Zhang, Sang Nguyen, Haiying Qin, Boro Dropulic, Daniel W Lee, Crystal L Mackall. CD22-targeted CAR T cells induce remission in B-ALL that is naive or resistant to CD19-targeted CAR immunotherapy. Nature Medicine, (2017);DOI: 10.1038/nm.4441
Source-Medindia
 MEDINDIA
MEDINDIA


 Email
Email