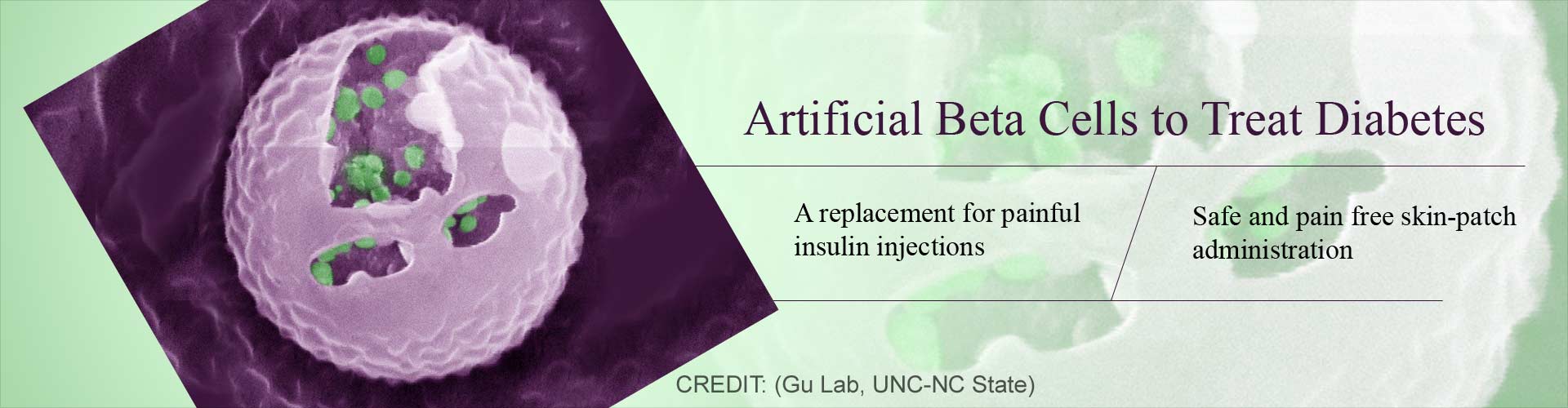
Newly developed artificial beta cells release insulin into the bloodstream automatically upon sensing an increase in glucose levels.
TOP INSIGHT
Artificial Beta Cells (ABCs) contain insulin filled vesicles that fuse with the outer membrane to release insulin when blood glucose levels rise.
Highlights:
- Artificial Beta Cells (ABCs) developed that mimic the pancreas’s beta cells that regulate insulin in the bloodstream.
- Newly developed ABCs automatically release insulin when an increase in glucose is sensed.
- In-vivo experiments using ABCs in diabetic mouse models were able to neutralize glucose levels and keep them at normal levels for up to 5 days.
Artificial Beta Cells
Beta cells are a group of cells within the pancreas that produce, store and secrete insulin. Insulin is the key regulator of glucose in the blood stream. Loss or dysfunction of the beta cells results in lack of production of insulin or production of non-functional insulin leading to diabetes. Artificial Beta Cells (ABCs) are synthetic cells that automatically release insulin into the bloodstream when there is an increase in the blood glucose levels . Although these cells are very different from the natural beta cells of the pancreas, they mimic the same functions. They are capable of sensing glucose levels, internally transducing signals and dynamically secreting insulin via vesicle fusion.How do ABC’s function?
The ABCs are constructed with a normal cell’s bi-lipid membrane. The key innovation in the ABCs are the insulin-stuffed vesicles. The synthetic beta cells function based on fusion-mediated insulin secretion. A rise in the blood glucose levels causes chemical changes in the coating of the insulin filled vesicles. This change leads to the fusion of the vesicle to ABCs bi-lipid outer membrane thereby releasing the insulin."This is the first demonstration using such a vesicle fusion process for delivering insulin that employs insulin-containing vesicles like those found in a beta cell and can reproduce the beta cell’s functions in sensing glucose and responding with insulin ’secretion’," said Zhaowei Chen, PhD, a lead author and postdoctoral researcher in the lab of Dr. Zhen Gu, the principal investigator and a professor in the Joint UNC/NC State Department of Biomedical Engineering.
Current treatment for diabetes
While there are several treatment measures available to maintain and control diabetes including periodic injections, insulin pills and mechanical insulin pumps, none are able to perfectly mimic the beta cells role in regulating glucose. More often than not, imperfectly regulated blood glucose levels lead to hypoglycemia (low glucose levels) which is associated with behavioral changes, brain damage and death. While cell therapy based on transplantation of beta cells does provide promising results, it is expensive and requires donor cells. Immunosuppression after the transplant is another factor that limits the procedure.ABCs on the other hand can be administered transcutaneously and replaced every few days or be administered as a disposable skin patch. In the study, the team reports that a single injection of the ABCs into diabetic mice normalized glucose levels and kept the levels normal for up to five days.
This is what Dr. Gu had to say about the future prospects of ABCs: "Our plan now is to further optimize and test these synthetic cells in larger animals, develop a skin patch delivery system for them, and ultimately test them in people with diabetes."
Reference:
- Zhaowei Chen, Jinqiang Wang, Wujin Sun, Edikan Archibong, Anna R Kahkoska, Xudong Zhang, Yue Lu, Frances S Ligler, John B Buse, Zhen Gu. Synthetic beta cells for fusion-mediated dynamic insulin secretion. Nature Chemical Biology, 2017; DOI: 10.1038/nchembio.2511
Source-Medindia
 MEDINDIA
MEDINDIA




 Email
Email