Acute cholecystitis may present as a cardiovascular disease and misdiagnosis may occur due to ECG changes and biomarkers suggestive of cardiac pathology.
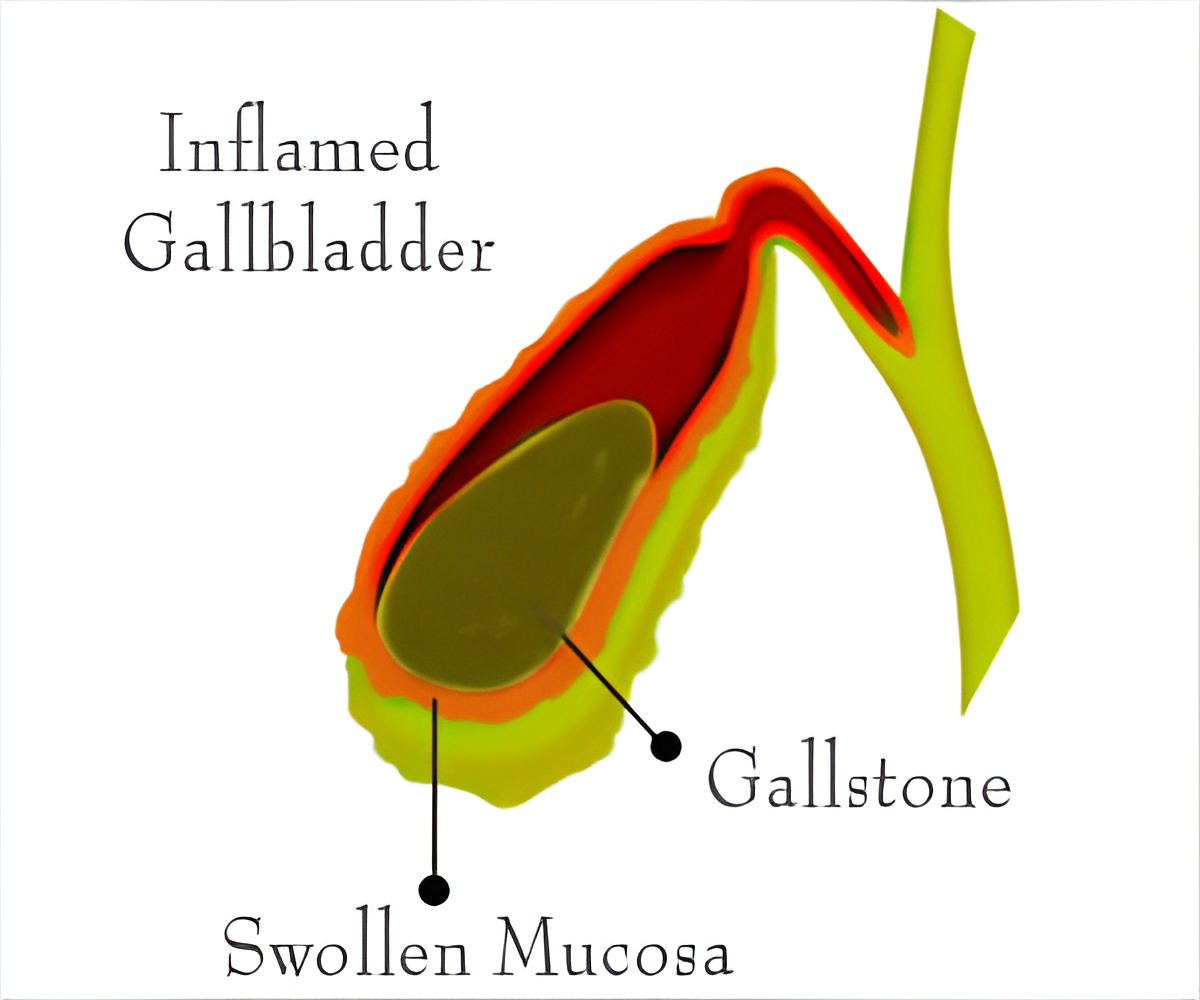
Group 1 – It comprised of 5 patients who were initially diagnosed with a cardiac event and were later found to have acute cholecystitis. Out of the 5 patients 4 came in with the complaint of chest oppression and were given an initial diagnosis of acute coronary syndrome while the remaining 1 patient came with complaint of loss of consciousness and was thought to have Adams Stokes Syndrome. Investigations showed that 2 of these patients had ECG changes, like T wave inversion and ST segment depression, which mimicked myocardial infarction, while the other 3 showed elevated biomarker levels H-FABP (Heart-type fatty acid binding protein) for myocardial injury. The final diagnosis was reached by symptoms of fever and abdominal pain, lab data suggestive of inflammation, negative results on coronary Angiography and positive results on imaging studies, all indicative of acute cholecystitis.
Group 2 – It comprised of 11 patients who showed both cardiac disease and acute cholecystitis, 2 of them having been diagnosed at the time of admission and 9 developing it de-novo. Aortic dissection was the most common coexisting condition involving 5 patients. They came with complaints of chest/back pain with fever (or) abdominal pain (or) Dyspnea. Some of them were diagnosed with acute cholecystitis due to an incidental finding on abdominal CT.
Treatment with antibiotics helped resolve the issue in 2 cases while the rest needed gall bladder resection.
Cardiologist who admit patient with ECG & biomarker changes of heart disease to the ICU, must remember that acute cholecystitis too can give rise to similar changes and requires a different management strategy. According to the researchers this condition has been confused with cardiac events on various occasions due to unusual ECG changes and biomarker levels. The explanation of this association is as follows:
- There has been an indication that prolonged ICU stay of patients of congestive heart failure may increase the risk of cholecystitis.
- Biomarker H-FABP also increases in pulmonary embolism and hepatic injury.
- ECG changes may occur due to:
- Distension of bile duct may decrease coronary flow.
- There might be a vagus mediated coronary vasospasm.
- There might be dehydration and electrolyte imbalance due to inflammation.
- There may be decreased contractility of the ventricles.
- There may be obstruction to the ventricular outflow (Pressure overload) due to conditions like aortic stenosis.
- There may be ventricular inflow obstruction due to conditions like mitral stenosis.
- There might be volume overload on the ventricles leading to inefficient pumping and increased demand.
- Arrhythmias may cause irregular heart beat which lead to improper functioning of the heart.
- Diastolic dysfunction may occur wherein the ventricles might not be able to pump sufficient blood in conditions like constrictive pericarditis.
The research still has many limitations. Abdominal CT scan or ultrasound scanning are not routinely done for all cardiac patients hence clinically silent cases of acute cholecystitis may have been missed. The cases which have developed cholecystitis after discharge have not been recorded. Also, it is a retrospective study with a small sample size and the surveillance of the hepatobiliary system has been incomplete.
References:
1. http://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-015-1790-8Davidson’s Principles & Practice of Medicine – 21st Edition
Source-Medindia