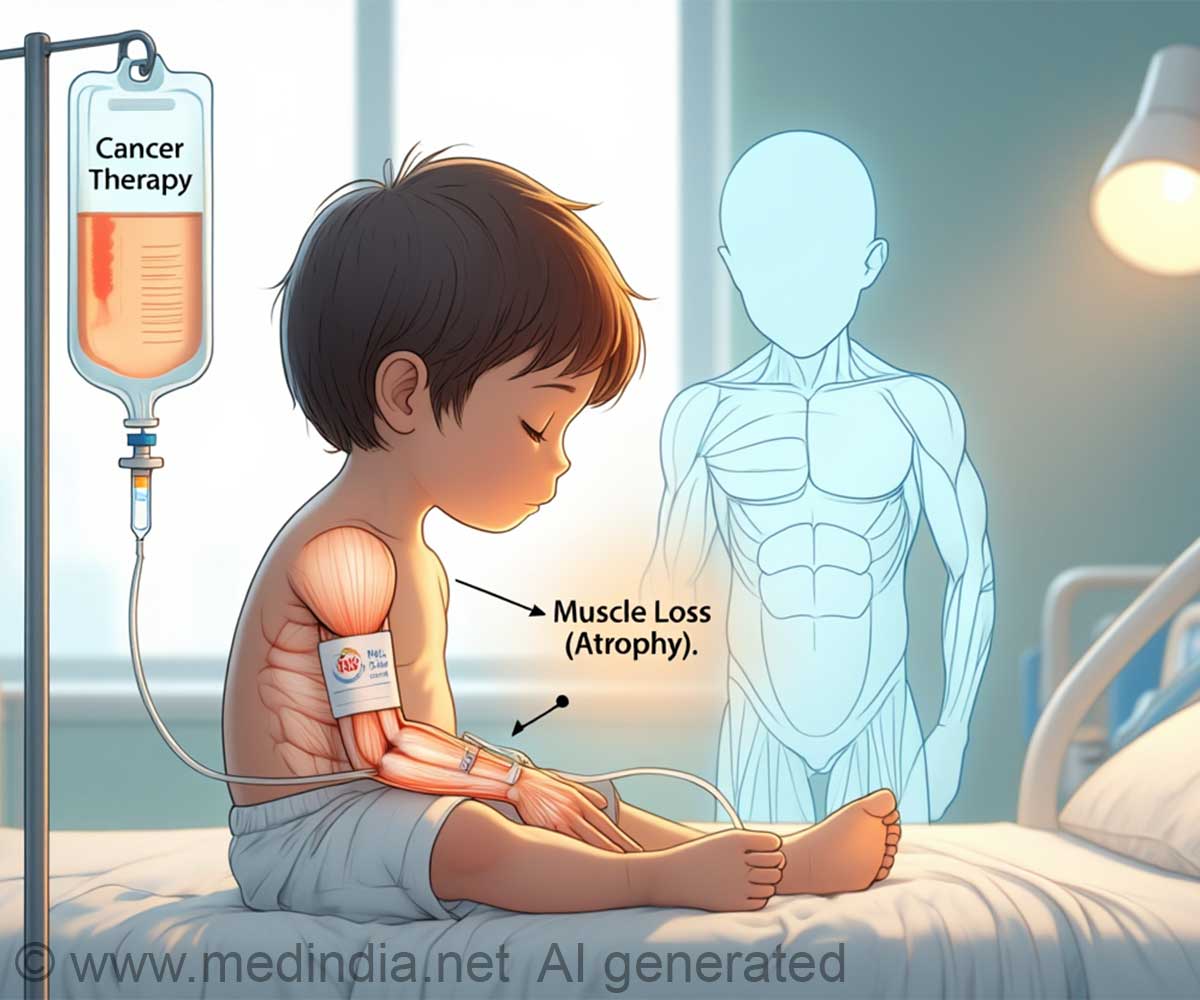
Muscle loss vs fat gain in pediatric oncology, alters drug dose precision and heightens the side effects, showing poor outcomes.
Longitudinal changes in skeletal muscle in children undergoing cancer treatment: a systematic review and meta-analysis
Go to source). Research from Edith Cowan University (ECU) shows that muscle loss triggered by both cancer and its treatment, may make kids less tolerant of chemotherapy. This impaired tolerance elevates drug toxicity risks, leading to worse outcomes and greater chances of lasting health complications.
TOP INSIGHT
Did You Know?
Children normally #gain_muscle of 3-5 Kg every year during growth spurts, but #cancer_treatment swipes this to #muscle_loss, raising metabolic-risks.
#pediatriccancer #muscleLoss #chemotherapy_sideEffects #fatmassincrease
Persistent Repercussions of Muscle Loss in Children
“Losing muscle also makes children and adolescents more vulnerable to heart and metabolic problems such as high blood sugar and insulin resistance,” Ms. Markarian said.“For example, during the onset of puberty children gain 3 kg to 5 kg of muscle per year. If treatment interrupts this growth and it isn’t recovered afterwards, it can severely impact health outcomes in the longer term.”
The research also found that children undergoing cancer treatment are likely to experience increases in fat mass, which can further contribute to metabolic problems and increase the risk of heart-related issues.
The Hidden Risk in Children’s Cancer Treatment
“Weight is not the whole story. Two kids can weigh the same, one with healthy muscle, one with excess fat, and their ability to tolerate chemotherapy could be very different.”“The challenge here is differentiating between muscle loss and fat gain, as this could have important clinical implications. Shifts in body composition can create a mismatch between dosing assumptions and actual metabolic capacity, heightening the risk of treatment-related complications and poorer clinical outcomes in patients with diminished skeletal muscle mass,” Ms Markarian said.
Reference:
- Longitudinal changes in skeletal muscle in children undergoing cancer treatment: a systematic review and meta-analysis - (https://link.springer.com/article/10.1007/s00431-025-06349-5)
 MEDINDIA
MEDINDIA


 Email
Email