Complement pathway drives red blood cell breakdown in sickle cell disease, revealing factors beyond genetic mutations.
Complement is activated in patients with acute chest syndrome caused by sickle cell disease and represents a therapeutic target
Go to source).
FDA-Approved Drugs Show Promise for Sickle Cell ACS
In preclinical models, the team demonstrated that blocking this pathway with existing FDA-approved drugs significantly reduced the severity of ACS symptoms. These findings, published in Science Translational Medicine, open the door to new therapeutic approaches that could dramatically improve outcomes for patients with sickle cell disease.TOP INSIGHT
#Redbloodcell breakdown can worsen #heart conditions. New understanding reveals complement activation causes #RBC lysis, triggering a feedback loop that may contribute to #AcuteChestSyndrome (ACS). #ResearchBreakthrough #SickleCellDisease
Sickle Cell Disease: Unraveling the Complement System's Role in Acute Chest Syndrome
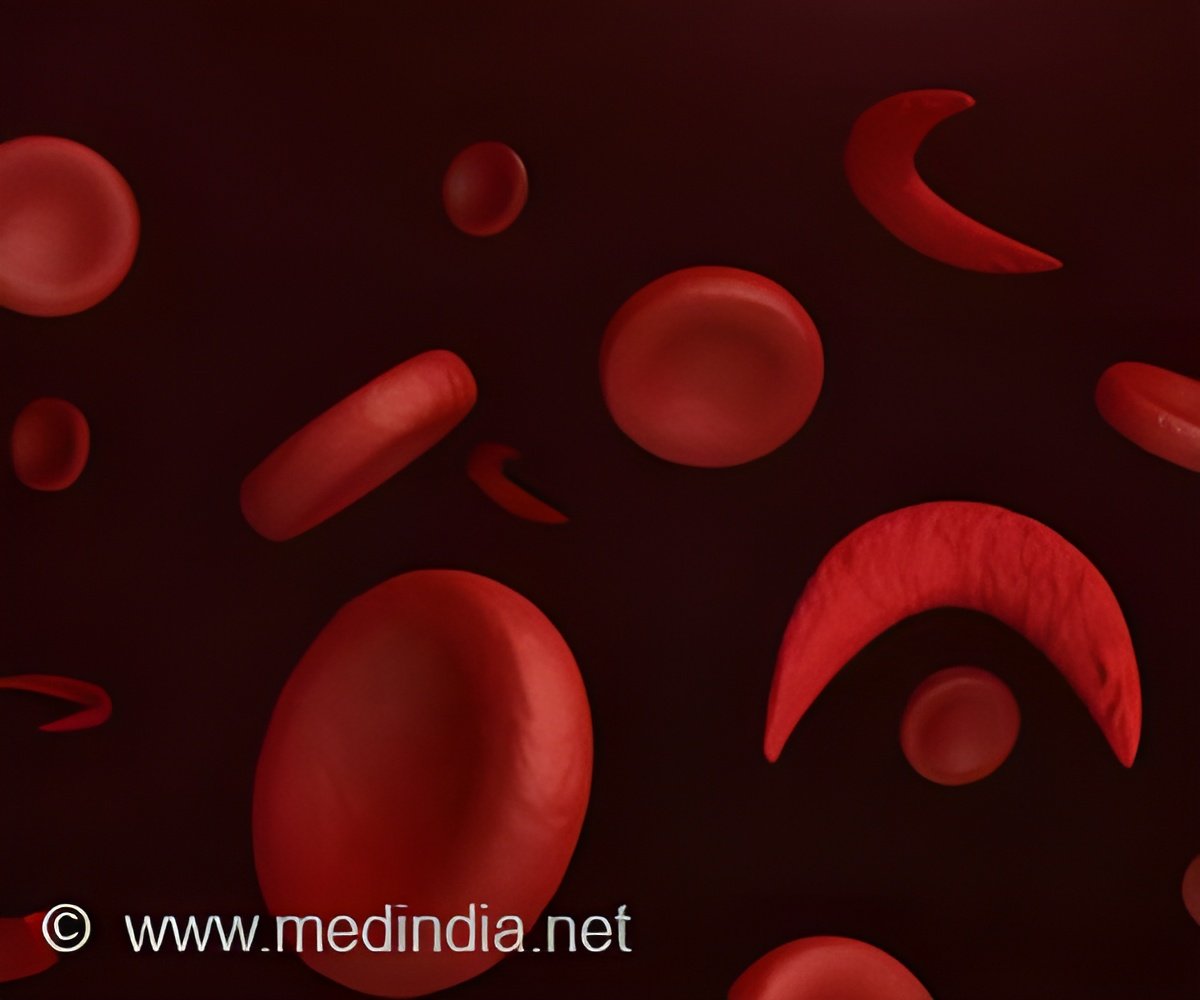
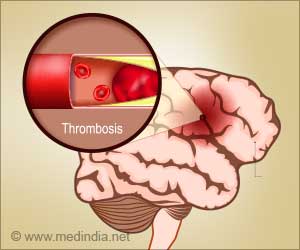
Sickle cell disease occurs due to an inherited mutation in hemoglobin that causes the destruction of red blood cells (RBCs), or hemolysis. This, in turn, can block blood vessels, injure the lungs, and eventually progress into ACS—a condition that includes shortness of breath, chest pain and wheezing that can quickly progress and turn fatal. Prior research has suggested that hemolysis can activate the complement system — a group of immune proteins that trigger a cascade of events to eliminate pathogens. However, it has been unclear how the complement system contributes to ACS and disease progression.The research team analyzed blood samples from 27 patients with sickle cell disease and detected higher baseline levels of complement activation when compared to healthy controls. They also observed increased complement activation in patients experiencing ACS. Using a mouse model of sickle cell disease, the investigators found that the complement pathway helped cause the breakdown of red blood cells, indicating that factors other than mutated RBCs may be contributing to the symptoms of sickle cell disease.
They also found that the breakdown of red blood cells caused by complement activation created a cycle of even more activation, which led to ACS. By removing certain complement proteins or using existing drugs to block them, researchers were able to reduce the breakdown of red blood cells and prevent ACS in their studies with animal models.
The authors propose that randomized clinical trials could be conducted to see if complement inhibitors that target different parts of the pathway could be effective in patients with ACS.
- Complement is activated in patients with acute chest syndrome caused by sickle cell disease and represents a therapeutic target - (https://www.science.org/doi/10.1126/scitranslmed.adl4922)
Source-Eurekalert
 MEDINDIA
MEDINDIA


 Email
Email






