What is Spinal Fusion?
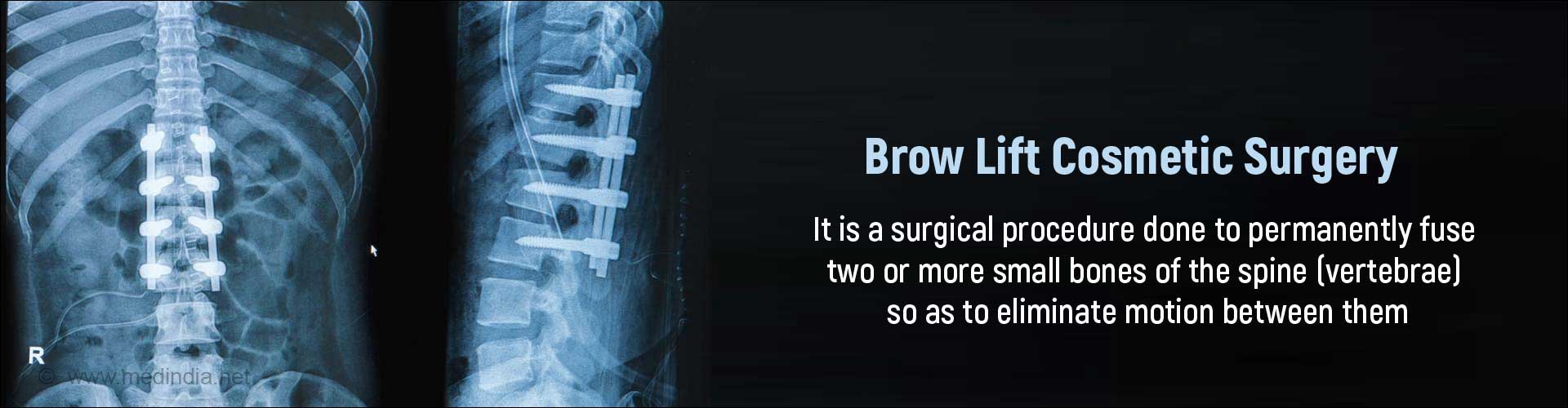
Spinal fusion is a surgical procedure done to permanently fuse two or more small bones of the spine (vertebrae) to make them into a single, solid bone so as to eliminate motion between them.
General Anatomy of the Vertebral Column
The vertebral column in humans consists of 33 vertebrae that are stacked one on top of the other and consist of 24 articulating vertebrae followed by the sacrum (which consists of 5 vertebrae fused into a single bone) and the coccyx (which consists of 4 fused vertebrae). The 24 articulating vertebrae are divided into 3 regions comprising of the cervical (7 in number), thoracic (12 in number) and lumbar (5 in number) vertebrae. The vertebrae are separated by intervertebral disks, which act as shock absorbers.
The spinal cord extends from the base of the skull to the lower back through a canal formed by an opening in each stacked vertebra. The spinal cord transmits information between the brain and the rest of the body through nerves that branch out through openings in the vertebrae.
When there is abnormal or excessive motion between the vertebrae, they compress the spinal nerves and cause pain. The reasoning behind spinal fusion is that the pain would stop if the bones do not move over each other.
Spinal fusion also prevents the stretching of nerves and surrounding ligaments and muscles. It is only recommended when the source of the pain has been detected accurately through imaging tests.
The surgery can be performed at all three levels of the spine; namely, the cervical, thoracic or lumbar regions. All techniques of spinal fusion involve bone grafting as the main part of the surgery. After some time, the bone graft and the vertebrae grow together and limit the motion at that segment, thereby relieving pain. The procedure is particularly useful in those with a significant loss of disc space height, deformity of the spine, and significant pain in addition to symptoms in the limbs.
Spinal fusion could partially restrict you from bending your back forward or backward. Although it does take away some spinal flexibility, most of the spinal fusions are performed only on small segments of the spine and do not limit motion much.
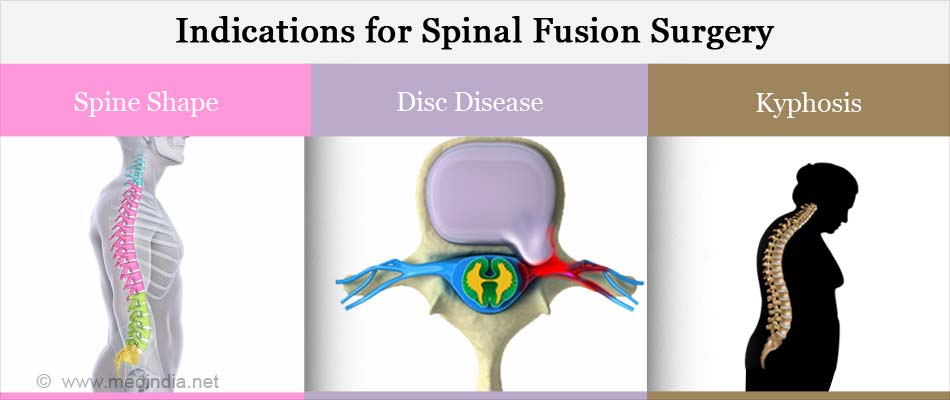
Why is Spinal Fusion Done?
Spinal fusion is performed for various reasons and in various situations. Decisions to perform it are made taking into consideration the:
- Shape of the spine
- Nature of disc disease
- Symptoms experienced by the patient
Spinal fusion is done along with other surgical procedures of the spine like decompression (foraminotomy or laminectomy) and after discectomy in the neck. The above procedures are done to remove bone and diseased tissues that narrow the openings through which the spinal nerves exit the vertebral column thereby putting pressure on the spinal nerves (spinal stenosis).
Spinal fusion is also done to relieve symptoms of many back conditions, including:
- Degenerative disk disease (when the disc or cartilage between two vertebrae wears out) to relieve pain and pressure on the spinal cord
- Spondylolisthesis, a condition when one vertebrae slips forward on top of another
- Arthritis of the spine
- Abnormal curvature of the spine like scoliosis and kyphosis
- Traumatic injuries or fractures to the bones of the spine
- Weak or unstable spine caused by infections, tumors or surgical decompression of the nerve
What are the Types /Approaches of Spinal Fusion?
To perform a spinal fusion, the surgeon can approach the bone from different angles depending on the nature and location of the disease. For example posterior fusion is generally considered the gold standard for spondylolisthesis and the preferred approach for an anterior lumbar interbody fusion (ALIF) is by making an anterior incision in the abdomen.
The spine can be approached from the
- Front or the anterior side; this usually requires an incision in the lower abdomen.
- Back / posterior side; in this procedure, you will be lying face down, and muscles and tissues will be separated from the back to expose the spine.
- Sides / lateral way if you are having surgery on your lower back. Tools called retractors will be used to gently separate, and to hold the soft tissues and blood vessels apart.
The spinal fusion technique also varies depending on the level of the spine affected and the location of the compressed spinal cord/nerves. It can be done at the cervical (neck), thoracic (mid-back) and the lumbar (low-back) regions of the spine.
- The cervical approach is through an incision in the front or the side of the neck. It can also be done through the back of the neck or through both, the front and back.
- The thoracic approach can be done through an incision in the chest and abdomen, or through the back, or both.
- The lumbar approach is mostly through an incision in the back though, it may also be done through the abdomen.
How do you Prepare for a Spinal Fusion Surgery?
Your doctor will examine you and conduct several tests to confirm the diagnosis and the need for the surgery. A CT scan or an MRI are commonly conducted to diagnose back problems:
For a CT scan, you will be asked to lie down still on a special table for a few minutes. A doughnut-shaped instrument will pass over the part to be screened, and images will be taken. A contrast may be injected into your vein; therefore you should inform the radiologist if you suffer from any allergies.
For an MRI, you will be placed inside a narrow tube, which can sometimes make you claustrophobic, if you have a fear of enclosed spaces. Few centres do offer more open MRI machines, but the drawback is that the pictures may not be as clear. The MRI machine makes loud clicking noises and it is advisable to ask for earplugs to help block these noises out.
Routine tests:
All patients who undergo an elective surgery (which is more planned), routine tests are required and include the following:
- Blood tests like hemoglobin levels, blood group, liver and kidney function tests
- Urine tests
- ECG to study the electrical activity of the heart
- Chest x-ray
In older group of patients, a detailed assessment of the heart maybe required.
A few preparations are required before a spinal fusion surgery; these are listed below:
Quit smoking: You will have to quit smoking well before the surgery since continuing to smoke before, during and after the procedure can affect the healing process. Smoking or inhaling tobacco smoke also irritates the breathing tubes and may reduce the function of your lungs during or after surgery.
Medicines: You will have to inform the doctor about the medicines you are taking, including herbs and supplements which you may take without a prescription. You will have to stop taking medicines that make it harder for your blood to clot two weeks prior to the surgery. These include drugs like aspirin and clopidogrel.
Keep underlying conditions under control: Any underlying conditions like diabetes, heart disease, or other medical problems, will have to be checked and kept under control by your regular doctor or the specialist you see for that condition.
Blood donation: Blood may be seldom required due to its loss sometime during the spine surgery; this can necessitate blood transfusion. Therefore, it is advisable to keep a stock of either the patient’s own blood or a matching blood type from friends, family or from a blood bank. The patient can donate his or her own blood (autologous donation) prior to the surgery in instalments, starting within four weeks and finishing at least seven days before the surgery. A technique called “cell-saver” is also present in some centers where the blood that is lost during the surgery is recycled and the red blood cells are given back to the patient.
Alcohol: Inform your doctor if you have been drinking a lot of alcohol.
Additional tests: The following tests might be required: Pulmonary or breathing function test to determine the lung’s capacity to expand, to see how much air you can breathe in and out. Scoliosis patients usually have difficulty breathing comfortably.
ECHO (echocardiogram) that takes a picture of your heart.
You will be advised medications to prevent constipation around a couple of days before the surgery, which will be continued during your hospitalization and for a few days after your discharge.
Apart from this, make sure you plan ahead for recovery at home post surgery.
- Get your home ready to ensure a safe environment after your discharge from the hospital; for example it will help you if you have railings on stairs and grab bars in the bathrooms.
- Check with the doctor if you will need any assistive devices after surgery like special shoes or aids to assist with walking.
- Ensure that there is a family member or a caregiver to support you during the first week after discharge.
Day before surgery: You will be instructed to avoid all food and liquid after midnight the night before the surgery. You will also be instructed about the medications you should take in the morning of the surgery with a sip of water. Check the recommended diet for the day before the surgery so as to limit the residue in the digestive tract.
What Happens During the Surgery?
On the day of the surgery
- An antibiotic will be given before the surgery that will be continued afterward to prevent any infections.
- Your health history and physical examination results will be reviewed.
- An IV (intravenous) line will be started through which you will receive medicines and fluids.
- Your operative site will be prepped and the surgeon will mark the site of surgery on your body.
- Your vital signs (height/weight, temperature, pulse, and blood pressure) will be checked, and you will change into a hospital gown.
Type of Anesthesia – Spinal fusion is done under general anesthesia during which time you will be unaware of the operation. Your anesthesiologist will decide on the options of anesthesia and pain medication after the surgery after reviewing your health history and physical exam results.

When you are ready to be taken to the operating room, you will be transported there.
Shift to the Operating room - The ambiance in the operating room can sometimes be very daunting and a small amount of sedation can help overcome your anxiety. From the trolley, you will be shifted on to the operating table. As you look up, you will see the operating light console and at the head end will be the anesthesia machine. There may also be monitors to check oxygen levels, ECG and other vital parameters. A constant beeping sound may be present from the monitors, which may sometimes be irritating.
The Operating Room (OR):
The anesthesiologist will start the pain medication. Pain control can be achieved through a patient-controlled analgesia (PCA) (a computerized pump with a tube of pain medication delivered through the IV line) or an epidural catheter that delivers pain medication directly to the spine.
You may also be asked to breath through a mask, which is also used to help you fall asleep.
Once you are asleep, a few tubes will be inserted into your body for various purposes:
- A small tube that is inserted in the back of your mouth and throat and into your airway to deliver oxygen to your lungs during surgery. This is usually removed before you wake up after surgery.
- A nasogastric tube (NG tube) that goes in through the nose and down into the stomach to prevent nausea and vomiting may be used sometimes. This tube is usually removed only on the 2nd or 3rd postoperative day.
- A Foley catheter into your bladder to drain urine from your bladder so that it can be measured and monitored post-operatively. The catheter is usually removed on post-operative day 2 or 3.
Procedure:
First, the doctor makes a surgical cut (incision) to view the spine. Spinal fusion is mostly performed after other surgeries such as diskectomy, laminectomy, or a foraminotomy.
Bone grafting: All spinal fusions require some type of bone material like a bone graft or artificial bone substitute to be packed between the vertebrae in order to bridge the gap and to help them heal together. The bone material can be
- A piece of bone 1-2 inches in length obtained from another part of the body, usually the pelvis or the leg bones of the patient (autograft). A small cut is made over the hip to remove some bone from the backside of the rim of the pelvis. Thus, autografts have the disadvantage of an additional incision that also lengthens surgery time and increases pain after the operation.
- A bone obtained from a donor / bone bank (allograft) which is a cadaver bone.
- An artificial / synthetic bone substitute. A few types are listed below:
- Demineralized bone matrices (DBMs) are made from cadaver bones from which the calcium has been removed. They are usually combined with other grafts; their protein content may help in bone healing.
- Bone morphogenetic proteins (BMPs) are very powerful synthetic bone-forming proteins that promote a solid fusion and can be used in certain situations.
- Ceramics are synthetic calcium/phosphate materials that are similar in shape and consistency to autograft bone.
The bone graft stimulates bone healing by increasing bone production and makes the vertebrae heal into one solid bone.

The different ways of fusing the vertebrae together are:
- Placing strips of bone graft material over the back of the spine
- Placing bone graft material between the vertebrae
- Placing special cages (packed with bone graft material) between the vertebrae
Immobilization:Following bone grafting, the vertebrae need to be held together to help the fusion progress. It is common in today’s surgeries to supplement the bone graft with additional hardware like screws, plates, and rods. This is called internal fixation. They have higher union rates than non-instrumented fusions and are often used to hold the bones in place without moving while the graft fuses the two vertebrae together. Internal fixation helps to move about earlier after surgery.
Minimally invasive techniques are also gaining popularity. These allow rods and screws to be inserted into the spine with smaller incisions with the help of advanced image guidance systems. They have the advantages of less muscle damage, blood loss, infections, pain, and length of stay in the hospital.
What Happens After the Procedure?
Waking up from Anesthesia –Once fully awake, you will be shifted on the trolley and taken to the recovery room, where a nurse will monitor your vitals and observe you for an hour or two before shifting you to the room or a ward.
Post-operative recovery:
- Spinal fusion requires you to stay in the hospital 3 to 4 days after surgery.
- Medicines to curb pain will be given via an intravenous line (IV) and through mouth or as a shot a couple of days after surgery. You will be prescribed painkillers to take after your discharge.
- You will be given instructions on how to control your movements including how to sit, stand, and walk.
- You will need to use a "log-rolling" technique when getting out of bed, a technique that involves moving your entire body at once, without twisting your spine.
- You may find it difficult to eat for 2 to 3 days during which time nutrients will be given intravenously.
Recovery at home:
- When you leave the hospital, you may need to wear a back brace or cast. Braces limit motion in the surgical area and thus help with the bone fusion growth. New bone formation usually takes from 3 –12 months.
- If you have undergone a low or mid-back surgery with fusion, braces are required at all times after the surgery except when you are in bed.
- If you have undergone a neck surgery with fusion, you will have to wear a cervical collar for 6 weeks or more after the surgery.
- Your nurses and therapists will help you with proper bed mobility, transfers, walking, body mechanics, bathing and dressing techniques, and safety.
- Follow instructions and get trained by your health care provider on how to take care of your back at home after spine surgery.
What are the Risks and Complications of Spinal Fusion Surgery?
Potential complications are possible with any surgery. Please discuss them in detail with your surgeon prior to undergoing the procedure. Complications that may occur following spinal fusion surgery are as follows:
- Reactions due to anesthesia
- Infections at the site of the wound or vertebral bones
- Recurrence of original symptoms
- A condition called pseudoarthrosis where there is not enough bone formation. This is more common is people who smoke. If this occurs, a second surgery may needed in order to obtain a solid fusion
- Persistant pain at the bone graft site
- Spinal nerve damage causing weakness, pain, loss of sensation, and bowel or bladder problems. These complications are very rare
- Bleeding, which is expectedto a certain extent, but this is not typically significant
- Wearing away of the vertebrae above and below the fusion, leading to more problems later
- Blood clots, whichcan rarelyform in the legs and could break off and travel to the lungs causing pulmonary embolism
What is the Outlook or Prognosis for a Spinal Fusion Surgery?
Spinal fusion is not likely to take away all your pain especially if you have had chronic back pain before the surgery. Since the area that was fused can no longer move, the areas above and below are more likely to be stressed when the spine moves. This could result in future spine problems.
Weight reduction and exercising with definitely help in recovery.
 MEDINDIA
MEDINDIA
 Email
Email








