What Is Laryngectomy?
Laryngectomy is a surgical procedure performed to remove the entire larynx or parts of it under general anesthesia. Surgical voice restoration procedures are performed on patients undergoing total laryngectomy to enable them to communicate verbally.
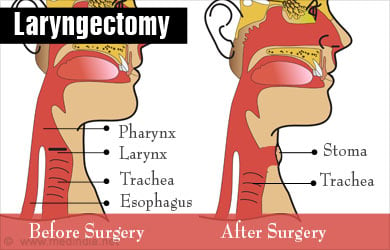
The larynx or the voice box is the mucous membrane lining part of the windpipe, present in between the esophagus and the nasal passages. It performs many important functions in the body.
- Sound production
- Swallowing
- Breathing
As verbal communication is an important aspect of daily life, a healthy voice box is sought after by singers, television anchors, radio jockeys and everyone else who likes to talk.
When the larynx is damaged or infected extensively, it would have to be partially or fully removed using laryngectomy.
Why Is Laryngectomy Performed?
Laryngectomy is performed when the patient is identified with,
- Advanced stages of throat cancer
- Severe trauma to the larynx
- Radiation necrosis as a result of radiation therapy
A large number of throat cancer incidents occur due to smoking tobacco or chewing tobacco.
What Are the Pre-Operative Guidelines?
There are certain guidelines to be followed prior to the surgery:
- Routine blood tests need to be taken along with physical examination by the doctor to ensure that the patient is fit enough for the surgery
- The doctor should be informed if the patient is pregnant
- Blood thinners like aspirin should be avoided for a few days before surgery
- Smoking should be completely stopped

- The patient should not eat or drink anything from midnight prior to the day of surgery.
- A nutritionist should be consulted to ensure ideal diet and nutrition after surgery
How is Laryngectomy Performed?
The patient is administered with general anesthesia and a small incision is made in the neck of the patient. The larynx and the associated lymph nodes are removed. If the pharynx is also affected by cancer, then the whole pharynx or parts of it are removed depending upon the extent of spread. Cancerous nodes, if present, are also surgically removed.
After the removal of the larynx, a small hole is made in the neck, the size of a small coin, and this facilitates breathing. This hole is called the stoma and it will never be removed. The skin is sealed back and drains are fixed, which will remain for a few days after surgery to help drain excess fluid.

Post Laryngectomy Rehabilitation for Voice
Once the larynx is removed, the patient will be unable to speak due to an inability to push air from the lungs to the mouth for speech. The patient would have to re-learn methods of communication and this will take time and patience. A speech therapist should be consulted for effective strategies and supportive measures.
To maintain a good quality of life, it is essential to open communication lines and start therapy based on the extent of surgery. Patients are often encouraged to carry notepads or laptops that can be used to write and maintain contact with the rest of the world. This is especially true if the patient is in need of something urgent and finds it difficult to pass on information using hand actions.
There are three methods of post-laryngectomy restorative therapies that will aid in near normal speech and help maintain the same quality of life.
- Tracheoesophageal Puncture (TEP)
- Esophageal speech
- Electrolarynx
These procedures will instill confidence in the patient after laryngectomy and empower them to feel independent.
What is TEP?
This is one of the most common methods of voice restoration in a patient who has undergone laryngectomy. This procedure cannot be performed on everyone and the doctor needs to asses and certify if it can be performed.
Highlights of TEP
- Only 25% of laryngectomy patients are eligible for this procedure
- Hands are not required during speech-rendering if hands-free
- The stoma is closed during speech
- TEP method is not effective for patients with
- Chronic obstructive pulmonary disease (COPD)
- Dementia
- Radiation therapy that exceeds 6,500 cGy
- Malnutrition
- Diabetes

TEP may be performed after the larynx is removed during a laryngectomy or may be performed a few days after. In this procedure, a small incision called the fistula is made to the back of the stoma, connecting the wind pipe and the esophagus. A voice prosthetic box is placed in the hole. Alternatively, a catheter may be inserted to keep the hole open. If it is not inserted in the fistula, then a catheter would have to be inserted via the nose for a few days to drain fluids.
The voice prosthesis functions by pushing air from the lungs to the moth via the voice prosthetic valve. This aids in speech. There are two types of TEP voice prosthetic boxes:
- Hands-free: The hands need not be used for speech
- With hands: The stoma has to be closed using the patient’s hands for the voice to be heard.
Not all patients are eligible for a hands-free device. Initially the muscles in the windpipe will be weak and communication may seem hard. However, over practice and as the muscles strengthen up, it will be easier to communicate.
Care for the Valves
The type of care depends on the type of valve used. If the valves used are external valves, then they need to be removed periodically and cleaned. If the air passages in the valves are blocked then will not allow the free passage of air, blocking communication. Initially a nurse or a trained assistant will guide the patient on how to remove the valve, clean it and then place it back in position. Once the patient is confident, the valve can be routinely cleaned by the patient at home.
Internal valves need to be changed once in every 6 months and this can be performed only by the doctor or the nurse and would require prior appointment.
Complications That Can Affect Speech After TEP
- Acid ingestion: Acid ingestion can result in swelling around the valves that can affect speech. To overcome this, doctors usually prescribe anti-acid pills that will prevent acid reflux.
- Spasms: Muscles spasms around the valve also restrict the flow of air and impair speech. Injecting botulinum toxin (BOTOX) will help ease the muscles and promote speech.
What is Esophageal Speech?
Esophageal speech was the most commonly used method of voice restoration after laryngectomy before the advent of the voice prosthesis. In this method of speech, air is pushed in from the food pipe and as the air travels down the throat it creates vibrations that produce sound. The mouth has to be moved just like in normal speech.
This method of speech requires a lot of practice though some people master it very fast. Some people, though, find it very hard and require help from speech therapists. The advantage of this method is that there are no devices or valves that need to be implanted and it is completely natural.
What is an Electrolarynx?
An electrolarynx is a device that is used to aid in speech if,
- The patient is not eligible for a TEP
- The patient did not opt for a TEP after a laryngectomy
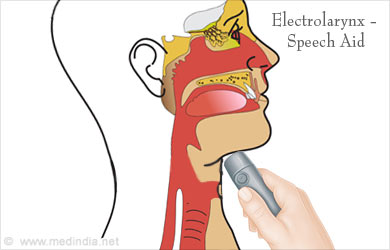
The device is the size of an electric razor and produces a sound when placed near the throat or via a tube placed in the mouth. Speech is carried out by moving the mouth and tongue just like in normal speech when the device produces the sound.
Initially the speech seems mechanical but over time and practice it is easier to communicate.
Table: Comparison between TEP, Esophageal Speech and Electrolarynx
| TEP | Esophageal Speech | Electrolarynx | |
| Process | Air from the trachea is pushed into the pharynx | Air pushed into the esophagus resulting in the vibrations in the throat | Mechanical sound that is adapted into the patient’s vocal tract |
| Efficiency | Between 40 to 90 % | Between 5 to 30% | Nearly 100% |
| Cost | Comparatively high | Nil | Low |
| Sound | Natural | Natural | Mechanical and loud |
| Training | Easy to be trained | Tricky | Requires a little effort |
| Disadvantages | Acid reflux, difficult to maintain | Longer periods of learning, difficulty in clarity | Its not hands free, requires batteries |
Apart from the prosthesis that are inserted to aid in speech, there are other flap surgeries that are used to improve communication. These surgeries are relevant during partial laryngectomy when the complete larynx is not removed and only parts of the larynx are removed. Types of flap surgeries include:
- Free flaps: Muscles from parts like the arm and the intestine are used to create flaps for reconstructing the larynx.
- Myocutaneous flaps: The muscle and the skin from the chest or other areas that are close to the throat is used to reconstruct the throat.
What Are the Risks Involved in Laryngectomy?
There are certain risks involved in laryngectomy:
- Stomal stenosis: The stoma could become tight resulting in stomal stenosis
- Inability to swallow well or to speak
- Pharyngocutaneous fistula: The tissue connection between the pharynx and the skin may not be formed leading to complications. To overcome this, Mahumut Denize and colleagues have stated in their paper titled “Pharyngoesophageal suturing technique may decrease the incidence of pharyngocutaneous fistula following total laryngectomy” that the use of Cushing type continuous suturing will reduce incidences of pharynocutaneous fistula
- Infection at the site of infection
- Hematoma: Accumulation of blood
- Allergy to any of the drugs used during the procedure
Current Research
Scientists are trying to culture glottis cells in the laboratory, which could pave the way for growing the larynx. However, current research is only in the initial stages.
Health Tips
The following health tips will help reduce the risk for throat cancer,
Eat Plenty of Colorful Fruits And Vegetables: The vitamins and minerals present in the differently colored fruits and vegetables will reduce the risk for throat cancer.

Quit Smoking or Chewing Tobacco: Tobacco smoking and chewing are one of the leading causes of throat cancer and should be completely avoided. There are dramatic positive changes to the body within a few weeks of quitting smoking
Stay Safe from HPV: Some forms of throat cancer are thought to be caused by the Human Papilloma Virus (HPV), which is a sexually transmitted virus. Therefore protection is essential to prevention.
Drink only Moderate Amount of Alcohol: Alcohol is another factor that can increase risk of throat cancer. Men should restrict themselves to two drinks a day and women to one.








