- Hashimoto's Disease - (https://www.niddk.nih.gov/health-information/endocrine-diseases/hashimotos-disease)
- Ajjan RA, Weetman AP. The pathogenesis of Hashimoto’s thyroiditis: Further developments in our understanding. Horm Metab Res. 2015;47(10):702-710.
- Caturegli P, et al, Hashimoto thyroiditis: Clinical and diagnostic criteria, Autoimmun Rev (2014) - (https://pdfs.semanticscholar.org/52a9/231787f489dc2cfa6a5caa1196fae086b9d2.pdf)
- Hashimoto's Disease - Symptoms and Causes - (https://www.mayoclinic.org/diseases-conditions/hashimotos-disease/symptoms-causes/syc-20351855)
- American Thyroid Association. Hashimoto's thyroiditis (Lymphocytic thyroiditis). - (https://www.thyroid.org/wp-content/uploads/patients/brochures/hashimoto_thyroiditis.pdf)
- Thyroid - Hashimoto's disease - (https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/thyroid-hashimotos-disease)
What is Hashimoto Thyroiditis?
Over a century ago (105 years to be precise), Dr. Hakaru Hashimoto first observed inflammation of the thyroid gland in 4 Japanese women. At the time, the term given to the condition was struma lymphomatosa or lymphadenoid goiter. The condition was very rare until the 1950s but was later found to be a common autoimmune inflammation (swelling) of the thyroid gland. The immune system (lymphocytes) infiltrates the thyroid gland and attacks the cells of the gland. The thyroid is an essential gland located at the base of the neck and releases hormones that influence growth and the way the body breaks down energy.
What are the Risk Factors of Hashimoto’s Thyroiditis?
Gender
Women are 8 times more likely to develop the condition compared to men. Hashimoto’s thyroiditis (HT) is observed more commonly in women between the age of 40 and 60 years though men, children and younger women are also prone to the condition.
Ethnicity
Hashimoto’s thyroiditis (HT) shows a high rate of incidence among Caucasians as compared with Asians, Africans, and Pacific Islanders. Genes and environmental factors contribute to the differences in susceptibility. A large number of implicated genes need to be confirmed through repetitive studies. Environmental factors, such as dietary iodine, excessive hygiene practices, reduced dietary selenium, viral infections, anti- HIV medications, and anti-cancer medications can predispose an individual to HT.
Age
Increased age is also a risk factor for HT.
What are the Different Types of Hashimoto’s Thyroiditis?
Hashimoto’s thyroiditis (HT) can be classified as:
Primary: In primary HT, the cause of the condition is unknown. It is a common form of HT and comprises a clinical spectrum of 6 different forms:
- Juvenile form
- Classic form
- Hashitoxicosis
- Fibrous variant
- Painless (silent) thyroiditis
- IgG4-related variant
Primary HT can occur due to an associated autoimmune disorder or entirely on its own.
Secondary: A known cause can be attributed to the development of secondary HT, for example, anti-cancer medications, cancer vaccines, and antiviral medications (e.g. Hepatitis C antiviral medications).
What are the Causes of Hashimoto’s Thyroiditis?
Hashimoto’s thyroiditis is an autoimmune condition, which basically means the body’s immune system starts to recognize its own thyroid cells as foreign and begins to attack it.
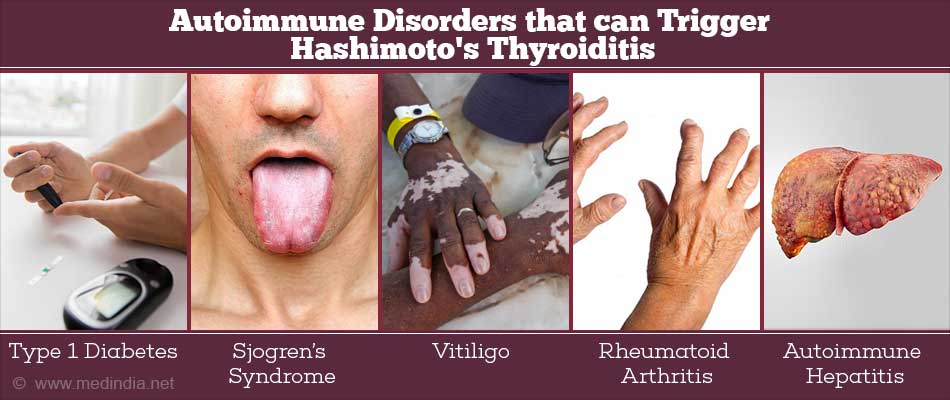
Other autoimmune conditions can also trigger the condition (primary HT). Some of these autoimmune disorders are:
- Type 1 diabetes
- Addison’s disease
- Sjögren’s syndrome
- Pernicious anemia
- Celiac disease
- Vitiligo
- Lupus
- Rheumatoid arthritis
- Autoimmune hepatitis
- Papillary thyroid cancer
A family history can also predispose individuals to suffer from Hashimoto’s thyroiditis.
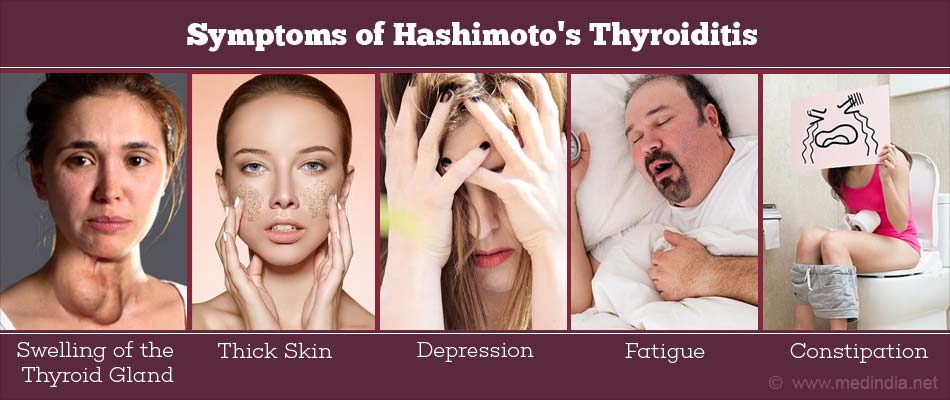
What are the Symptoms of Hashimoto’s Thyroiditis?
In the initial stages, there are no specific symptoms for Hashimoto’s thyroiditis. With disease progression, the thyroid starts to get swollen and enlarged resulting in goiter. As a result, the neck looks swollen in front. Since the thyroid gland gets damaged, there is a reduction in thyroid hormones and hypothyroidism sets in. However, in the early stages, hypothyroidism is not detected or is mild. Once the thyroid gland shrinks due to inflammation, the goiter disappears and the symptoms of hypothyroidism (listed below) become evident:
- Constipation
- Heavy or irregular periods
- Fatigue
- Weight gain
- Pain in muscles and joints
- Heartbeat becomes slow
- Dryness and thinning of hair
- Memory issues
- Inability to tolerate cold
- Depression
- Swelling of face
- Dry, yellow, cold, and thick skin
- Slow breathing
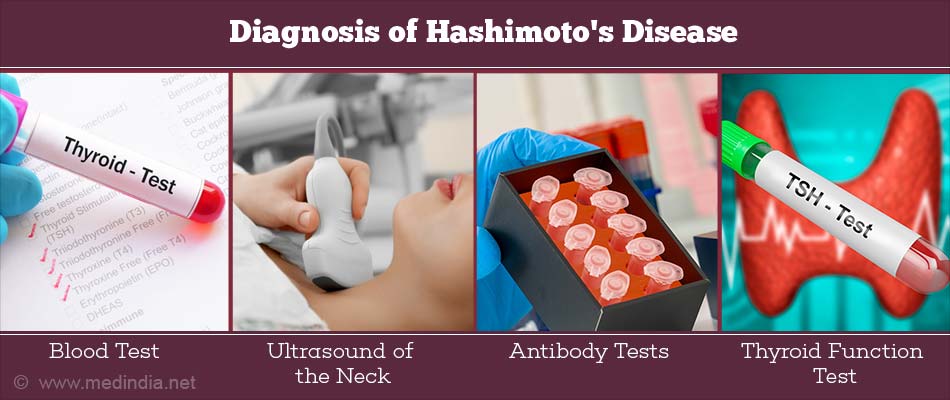
How do you Diagnose Hashimoto’s Thyroiditis?
As with any condition, the primary physician first takes the medical history of the patient which is followed by a physical examination.
Hashimoto’s thyroiditis can be diagnosed by a combination of clinical features, thyroid sonogram, and blood tests to detect antibodies against thyroglobulin and thyroperoxidase (TPO). Blood tests to detect thyroid hormone levels are also conducted.
1. Clinical features: There are local and systemic clinical features specific to HT
Local features:
- Difficulty in breathing
- Difficulty to swallow
- Hoarseness in voice
Systemic features:
- Swelling of the thyroid gland
- Hypothyroidism
Detecting antibodies
One of the main diagnostic tests is to check for antibodies against thyroperoxidase, a thyroid enzyme. Invariably, 95% of HT patients test positive for these antibodies
Another test is to detect antibodies against the major thyroid protein thyroglobulin. However, this test is not as sensitive as the anti-TPO test. Conventional practice estimates the antibody levels against both TPO and thyroglobulin
2. Ultrasound and fine needle aspiration
Neck ultrasound is an imaging technique to detect thyroid conditions, such as HT. If antibodies are not detected despite a strong suspicion of Hashimoto’s disease, then a thyroid ultrasound is performed, which can estimate the thyroid volume as well as the condition affecting the thyroid. In HT, there is reduced echo in the ultrasound. Thyroid ultrasound is also used to guide the insertion of the needle to obtain a fine needle aspirate. When a patient has nodules in the thyroid, fine needle aspiration is used to analyze the composition of the nodule.
Radio-iodine tests and thyroid function tests are other diagnostic tests that are used rarely.
How do you Treat Hashimoto’s Thyroiditis?
In the early stages of HT (normal thyroid hormones –TSH and thyroxine), the effects of hypothyroidism are not prevalent. Patients may be monitored on a regular basis. When hypothyroidism begins, the patient may be treated with an oral synthetic thyroid hormone medication called levothyroxine. A blood test is performed 6 to 8 weeks after taking the medication to monitor the thyroid hormone levels. If the levels stabilize then a blood test is taken only after 6 months or a year to monitor the progress with the medication. If the medication needs to be adjusted, then a blood test is again performed following 6 to 8 weeks to monitor the progress. The medication should be taken in the morning before intake of food.
If there is an excess dose of levothyroxine, then hyperthyroidism sets in while a reduced dose of levothyroxine results in hypothyroidism. Hence, an accurate dose of levothyroxine is necessary to maintain the normal functioning of the thyroid for life.
To treat IgG4-related variant of HT, glucocorticoids are found to be effective and can prevent the lifelong use of synthetic levothyroxine.
Surgery is performed only if the enlarged thyroid gland causes other complications.

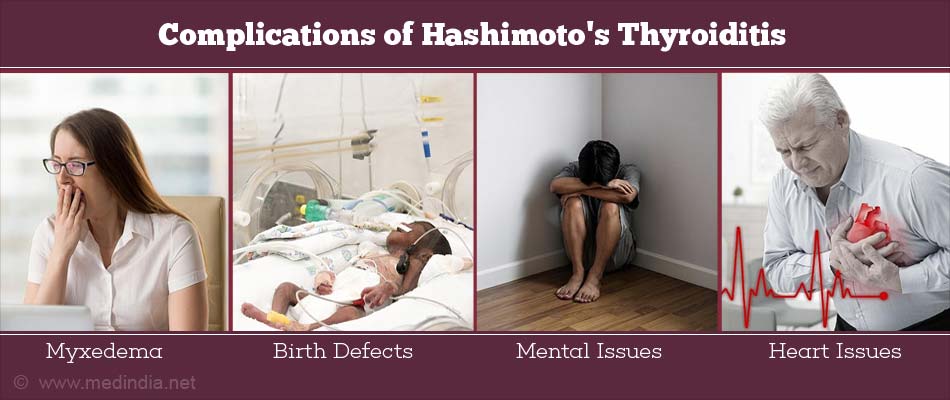
What are the Complications of Hashimoto’s Thyroiditis?
Hypothyroidism due to HT can give rise to numerous complications as listed below:
- Myxedema - Drowsiness, lethargy and unconsciousness
- Goiter
- Birth defects - Babies born to hypothyroid mothers have developmental and mental defects
- Mental issues - Depression, mental acuity issues, reduced sexual libido
- Heart issues - Enlarged heart and heart attacks result due to increased levels of low-density lipoprotein (LDL)
 MEDINDIA
MEDINDIA
 Email
Email