Stroke survivors residing in regions below standard housing conditions face a twofold increase in the risk of stroke.

American Heart Association
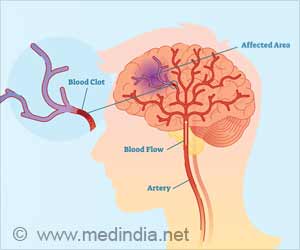
Go to source). The researchers found that among 2,164 people with ischemic (clot-caused) stroke, the one-year unadjusted risk of poor outcomes was 35 percent, 40 percent, and 46 percent for patients residing in neighborhoods with low, intermediate, and high deprivation, respectively.
TOP INSIGHT
Stroke survivors in areas with high unemployment, low income, poor education, and substandard housing quality are twice as likely to suffer poor recovery compared to those in more favorable conditions. #stroke #unemployment #education
"As a clinical research associate, I get to interact with them far beyond the completion of their urgent treatment, which sparked my interest in exploring the long-term outcomes for these patients,” she added.
Impact on Stroke Survivors' Recovery
In this study, researchers used data from Yale’s Longitudinal Study of Acute Brain Injury and Area Deprivation Index (ADI) rates for the 2020 US Census blocks to compare outcomes among stroke survivors by socioeconomic disadvantage factors.After considering the inability of the ADI to specifically measure each level of deprivation, the researchers discovered that those living in intermediate and high deprivation areas had 44 percent and 107 percent greater risk, respectively, of unfavorable outcomes, compared to patients living in neighborhoods with low deprivation levels.
Patients with poor outcomes were unable to manage their affairs without assistance and needed some assistance in daily activities.
Patients with good outcomes were able to live independently, although some still had residual symptoms, the researchers noted.
Reference:
- American Heart Association - (https://www.ahajournals.org/)
 MEDINDIA
MEDINDIA



 Email
Email










