New pain relief targets that could be used to provide relief from chemotherapy-induced pain have been discovered by King's College London researchers.

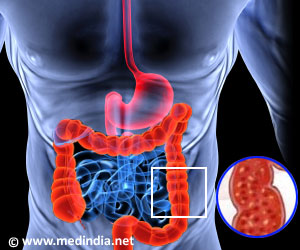
One potential side effect of some chemotherapy drugs (such as vincristine) is damage to nerves. This is particularly prominent in hands and feet as the drugs affect nerves in the periphery of the body. This causes pain which doctors treat with painkillers. However, some people find that the pain persists.
Dr Malcangio's team investigated why the chemotherapy drugs were causing pain in hope to solve the problem. The used mice in the study because mice given the chemotherapy drug also experienced pain in their nerve extremities (such as their hind-paws).
By studying the mice, they found that the pain was caused by the mouse's own immune system responding to damaged blood vessels.
Dr Marzia Malcangio explained: "The chemotherapy drug was found to cause damage to blood vessels around the nerves. When this happened, immune cells leave the blood flow and enter the nerve to help reduce the inflammation, but they also activate pain. Chemicals released naturally by the immune cells were activating the nerves and producing pain."
To try to prevent the pain, researchers looked at ways of stopping the immune cells entering the nerve. They identified receptors on the outside of the immune cells that could be targeted to stop their exit from blood, constituting new types of pain treatment.
Advertisement
Professor Jackie Hunter, BBSRC Chief Executive said: "This BBSRC CASE studentship has enabled a mutually beneficial research collaboration between academia and industry. Understanding the biological mechanisms of pain, using this mouse model, could lead to new types of pain management."
Advertisement