Intratumoral differences or heterogeneity can be blamed for chemo-resistance in small-cell lung cancer patients, finds a new study.

‘Further understanding of small cell lung cancer affecting intratumoral heterogeneity (ITH) is important to identify populations of cells that may drive certain pathways associated with aggressive resistance to chemotherapy.’





The challenge in studying why and how SCLC chemoresistance occurs is due to the fact that most patients do not undergo another biopsy or surgery at the time of cancer recurrence. This leaves investigators like Byers and Stewart with few SCLC samples with which to conduct genomic and biomarker analyses of drug-resistant tumors.To overcome the lack of SCLC samples, the team developed novel disease models by isolating circulating tumor cells from a simple blood draw. The cells, placed under the mouse’s skin, develop tumors representative of the patient from whom they were derived.
These SCLC models, called circulating tumor cell-derived xenografts (CDX), are unique to each patient and provide an opportunity to assess treatment response to novel targeted therapies, as well as changes that may occur in response to therapy.
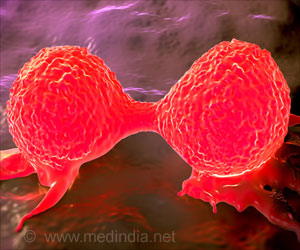
"We hypothesize that differences in gene and protein expression between tumor cells, called intratumoral heterogeneity, contribute to the rapid development of platinum chemotherapy resistance," said Stewart. "This means that there are likely multiple cell populations in SCLC patients who have not yet been treated. Some of those cells may be killed by chemotherapy but others will not. These resistant cells then continue to grow and prevent further response to treatment."
To study intratumoral heterogeneity (ITH) in SCLC, the investigators performed single-cell sequencing of CDX models to identify gene expression differences between individual cells from chemotherapy-sensitive CDX tumors compared to those that remain resistant.
Advertisement
SCLC has a variety of differences at the cellular and genetic level, from the way genes are expressed to which cell-signaling pathways are involved. These differences between tumor cells result in ITH. A more thorough understanding of ITH is important to identify populations of cells that may drive certain pathways associated with aggressive resistance to chemotherapy.
Advertisement
"Cells expressing each of these characteristics were identified across all tumors, suggesting cells sensitive or resistant to chemotherapy are both present in the same tumor," said Stewart. "However, even subtle shifts in the distribution of these genes can exert a significant impact on response to treatment."
Stewart adds that the team’s data support further use of single-cell analysis to explore the role of ITH in SCLC, including effects of treatment on cell populations.
"Through the use of these new mouse models, we report data that supports use of single-cell analysis to explore the role of ITH as a driver of drug resistance," said Stewart.
Source-Eurekalert