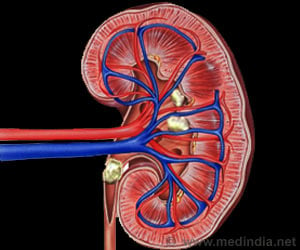
Sense of smell deficits are common, linked to malnutrition in patients with kidney disease. Olfactory function is impaired in patients with end stage renal disease.
TOP INSIGHT
Malnutrition is a well-known complication of chronic and end-stage kidney disease. Kidney disease patients often lose their interest in food due to unpleasant taste that may lead to malnutrition in renal disease patients.
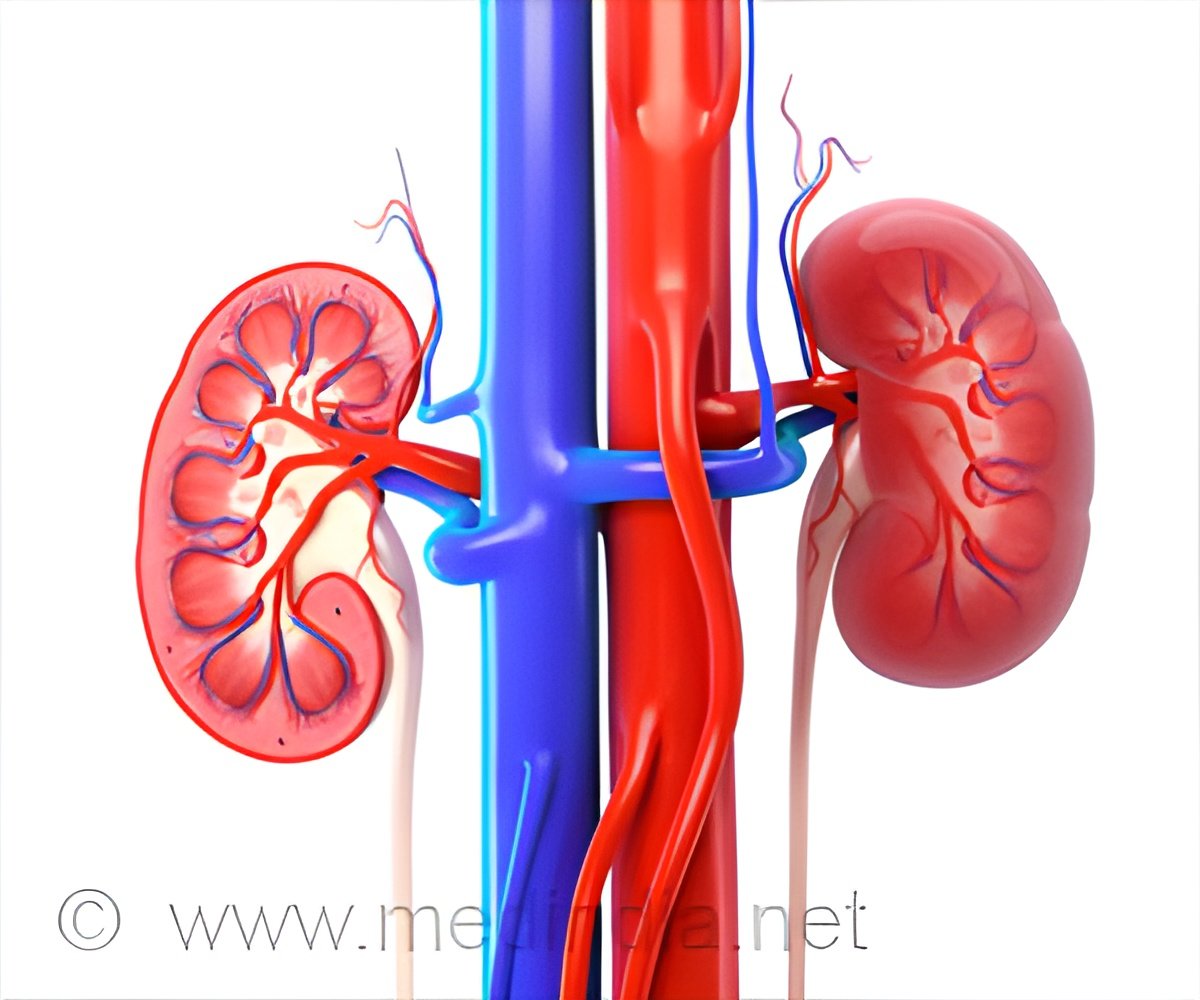
First author Sagar Nigwekar, MD, also of MGH Nephrology, explains, "More than 25 million adults in the U.S. have chronic kidney disease, with more than half a million requiring dialysis. Poor dietary intake leading to malnutrition is common in these patients, but there currently are no effective treatments addressing these complications. Establishing what these olfactory deficits are and how they influence patient nutrition is essential for the development of novel preventive or therapeutic interventions."
Kidney disease patients often lose their interest in food, reporting that it has a little flavor or an unpleasant taste, and the malnutrition that results is a significant contributor to worsening of symptoms and mortality risk.
Although several studies have reported impaired olfactory ability in kidney disease patients, others have had mixed results, and none have been the kind of large-scale assessment that could characterize how specific abnormalities influence nutritional status. As a result, even though the sense of smell has a major contribution to the flavors of foods, most efforts to increase food intake in kidney disease patients have focused on the sense of taste and direct appetite stimulation.
The current study enrolled 161 participants - 100 with end-stage kidney disease, all of whom were dialysis dependent; 36 with chronic disease not yet at the end stage, and 25 healthy controls. One test - the University of Pennsylvania Smell Identification test - determined participants' ability to identify specific odors.
Based on the odor identification tests, 69 percent of those with chronic kidney disease and 92 percent of those with end-stage disease had a significant reduction in their sense of smell. In the test determining odor detection thresholds, participants with end-stage kidney disease required a four times greater concentration of an aroma to be detected than did either those with chronic disease or control participants.
In all three groups, participants' nutritional status - determined by a standard assessment of food intake, weight changes and gastrointestinal symptoms, along with measures of factors such as cholesterol and albumin, which reflects protein metabolism - correlated with their olfactory abilities.
To test a potential treatment for these olfactory deficits, the team enrolled seven dialysis-dependent, end-stage kidney disease patients in a pilot study of theophylline - a drug approved to treat asthma and emphysema and previously reported to reduce such deficits in patients without kidney disease. Participants self-administered daily intranasal doses of theophylline for six weeks and had follow-up tests every two weeks during the study period.
While the odor identification scores of two participants deteriorated, for the other five they increased an average of 5 percent, with the greatest improvement in any participant exceeding 10 percent, compared with scores at the trial outset. For three participants, the improvement was enough to move them up one category, such as from severe to moderate loss of smell or from moderate to mild.
"We were very excited to find that the three patients in whom the odor detection threshold was improved by more than 10 percent after theophylline treatment were also the top three in terms of odor identification improvement," says Paunescu. "We know that in the general population olfactory deficits reduce the enjoyment of food and are risk factors for malnutrition, so the use of novel therapeutics to improve olfaction could be an innovative and effective way to prevent and alleviate malnutrition in kidney disease patients."
Nigwekar adds, "We're now planning to expand the investigation of olfactory deficits to a larger group of patients and determine whether or not poor dietary intake truly drives the association between olfactory deficits and nutritional quality.
A longer-term study should help us establish the sequence of events by which olfactory deficits lead to changes in food consumption and eventual malnutrition, and the encouraging preliminary findings of the theophylline trial warrant confirmation in a larger study." Both investigators are assistant professors of Medicine at Harvard Medical School.
Source-Eurekalert
 MEDINDIA
MEDINDIA



 Email
Email