Living implants, consisting of bone cells seeded on supporting structures (made of biological material) are used to promote bone repair.
‘The survival rates of bone cells increased when the oxygen sensor PHD2 was inactivated before implantation, which led to better bone regeneration.
’





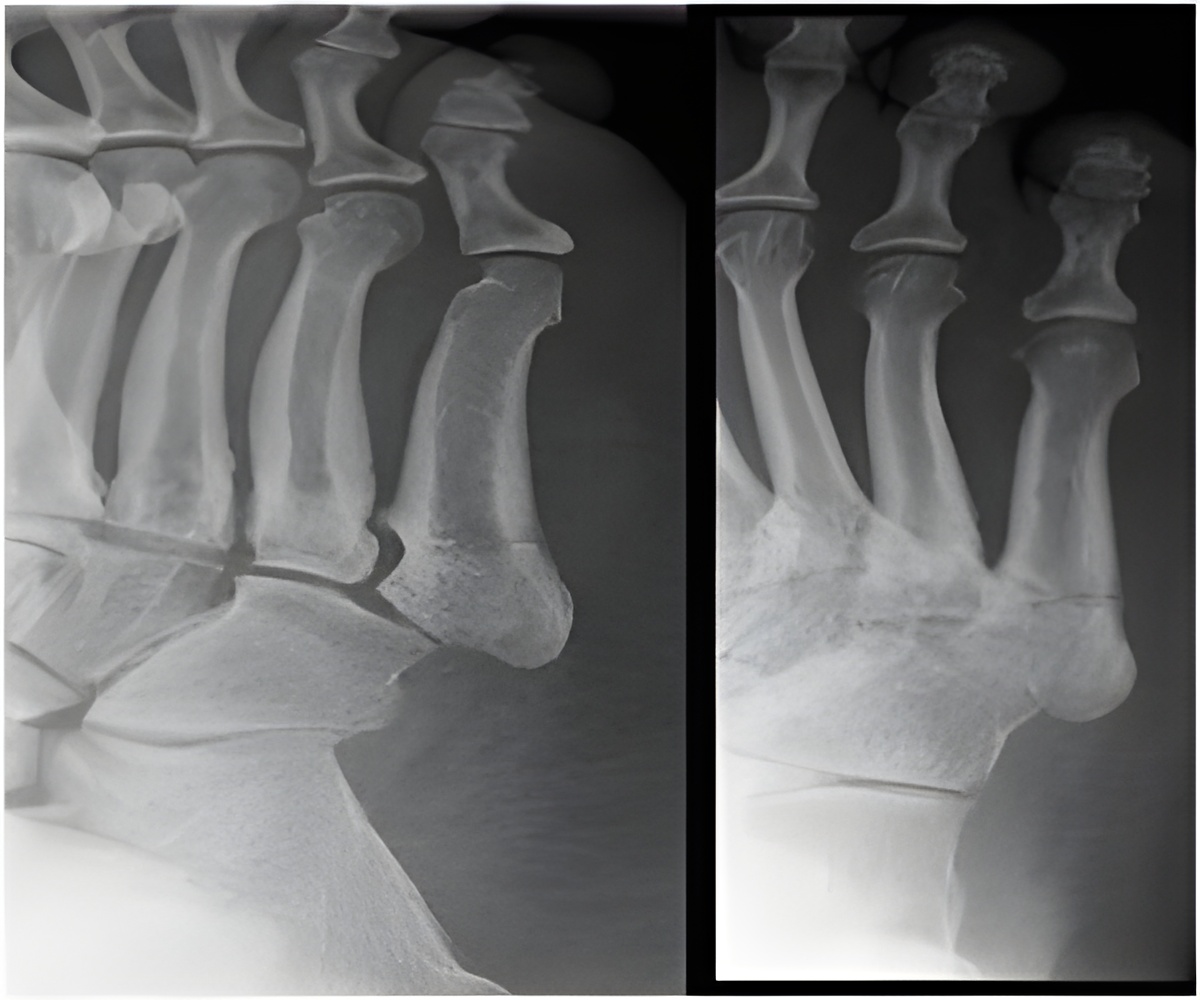
Unfortunately, many obstacles still need to be tackled before we have a functional living implant, explains Professor Geert Carmeliet of the Clinical and Experimental Endocrinology Unit. "Often, only 30% of the implanted bone cells will survive the first days. A major reason is that the blood vessels around the fracture, which deliver oxygen and nutrients to the cells, are also damaged. The ingrowth of new blood vessels into the implant takes time and until then, the cells are out of fuel since oxygen and nutrient supply is insufficient. At the same time, the starved bone cells produce harmful oxygen radicals and thereby disturb the natural balance between antioxidants and oxygen radicals. An excess of these oxygen radicals causes irreversible cell damage." Doctoral student Steve Stegen tested in mice how he could better equip the bone cells for that crucial stage between implantation and ingrowth of the blood vessels. He managed to switch on a survival mode in bone cells by inactivating the oxygen sensor PHD2 before implantation. "As a result, bone cells activate a dual defence mechanism. First, bone cells increase storage of an emergency fuel in the form of glycogen, which is in fact a sugar reservoir. In addition, bone cells start using glutamine -- an amino acid -- to produce more antioxidants to neutralize the increased production of harmful oxygen radicals. These two adjustments allow bone cells to be self-supporting in terms of energy generation and to protect themselves against an increased level of oxygen radicals."
The oxygen sensor PHD2 can be inactivated via genetic engineering, but, more interestingly for use in the clinical setting, also by administering therapeutic molecules, explains Professor Carmeliet. "Reprogramming bone cells obtained from patients might increase their survival rate from 30% to 60%, which will ultimately lead to better bone regeneration. In future research, we will examine whether this technique also works in even larger bone defects and by using human cells."
The findings are published in Cell Metabolism.
Source-Eurekalert