The importance of the neurotransmitter gamma-aminobutyric acid (GABA) in both Type 1 and Type 2 diabetes has been highlighted in two new studies. GABA is a naturally occurring neurotransmitter sending chemical messages through the brain and the central nervous system.
TOP INSIGHT
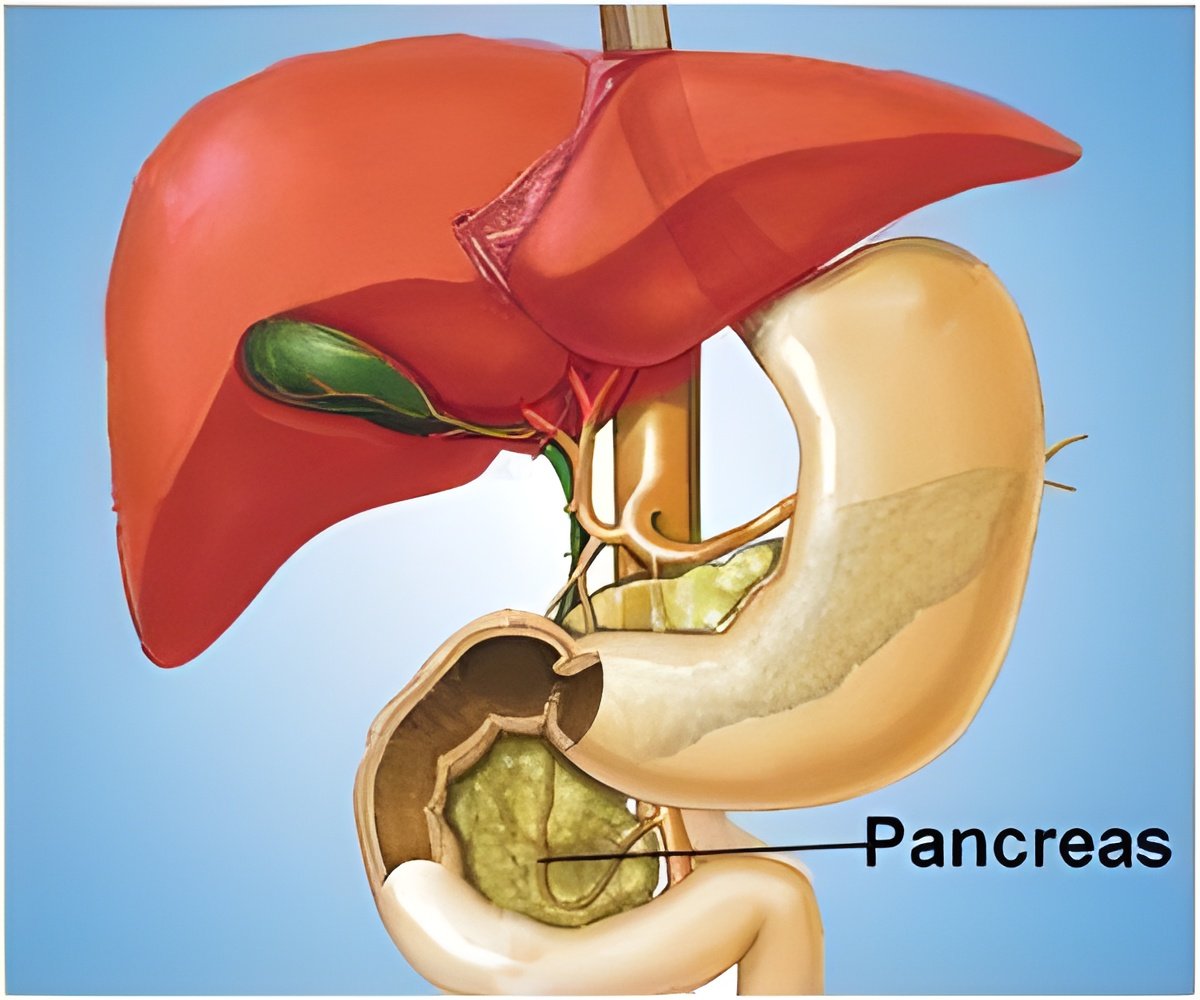
The anti-inflammatory effect of GABA or gamma-aminobutyric acid, a neurotransmitter, may be important in the pancreatic islets because, as long as GABA is present, toxic white blood cells can be reduced, thus increasing the survival of the insulin-secreting beta cells.
GABA is synthesized by an enzyme called GAD from the amino acid glutamate in nerve cells but also, importantly, in the insulin-producing beta cells in pancreatic islets. GAD has two forms, GAD65 and GAD67. In type 1 diabetes, beta cells are destroyed while type 2 diabetes is associated with impaired beta cell function and insulin resistance.
Patients with type 1 diabetes often have antibodies to GAD65. However, there has been no strong link between GABA and type 2 diabetes until recently when it was shown that GABA is important for maintaining and potentially also in the making of new beta cells.
The two current studies reinforce the image of GABA's importance, for both types of diabetes. The scientists used ion channels that GABA opens, the GABAA receptors, as a biological sensor for GABA, and were able to determine the effective, physiological GABA concentration levels in human pancreatic islets. They also showed that these ion channels became more sensitive to GABA in type 2 diabetes and that GABA helps regulate insulin secretion (Article 1).
The scientists then isolated immune cells from human blood and studied the effects GABA had on these cells. They show that GABA inhibited the cells and reduced the secretion of a large number of inflammatory molecules (Article 2).
In ongoing studies, the scientists now focus on clarifying the GABA signaling mechanisms in the immune cells and in the human beta cells. They will also study how existing drugs can increase, decrease or mimic the effects of GABA, says Bryndis Birnir.
Source-Eurekalert
 MEDINDIA
MEDINDIA




 Email
Email










