Extending the time between doses in people with rheumatoid arthritis in remission can be done in some patients without significantly increasing disease activity.
Once people with RA achieve remission, doctors often try to increase the interval between doses of drugs, which is called tapering, but doing so involves the risk of increasing disease activity and joint damage, reducing physical function, or causing a relapse. Researchers in France looked into how increasing the interval between injections of TNF-inhibitor drugs, which are both costly and may sometimes have serious side effects, might affect patients. They conducted an 18-month randomized, controlled trial involving 137 people with RA treated with biologic agents that inhibit TNF, who were in stable remission for at least six months. Seventy-eight percent of the participants were female, and all were using either etanercept (Enbrel®) or adalimumab (Humira®), for one year either alone or in combination with other drugs. Participants could be taking five milligrams or less of the corticosteroid drug prednisone daily.
Researchers split the participants into two randomized groups: One set using a progressive spacing out of injections of their TNF-inhibitor and one set who continued taking their injections at full doses at the approved time intervals. In the first group, doctors increased the time between two injections by 50 percent every three months up to a complete stop by the fourth interval. If the participants RA disease activity or physical function worsened, the patient stopped tapering doses of the drugs and was moved back to previous dose. To test the patient''s disease activity, function level and signs of relapse, doctors used standard scoring methods and health assessment questionnaires.
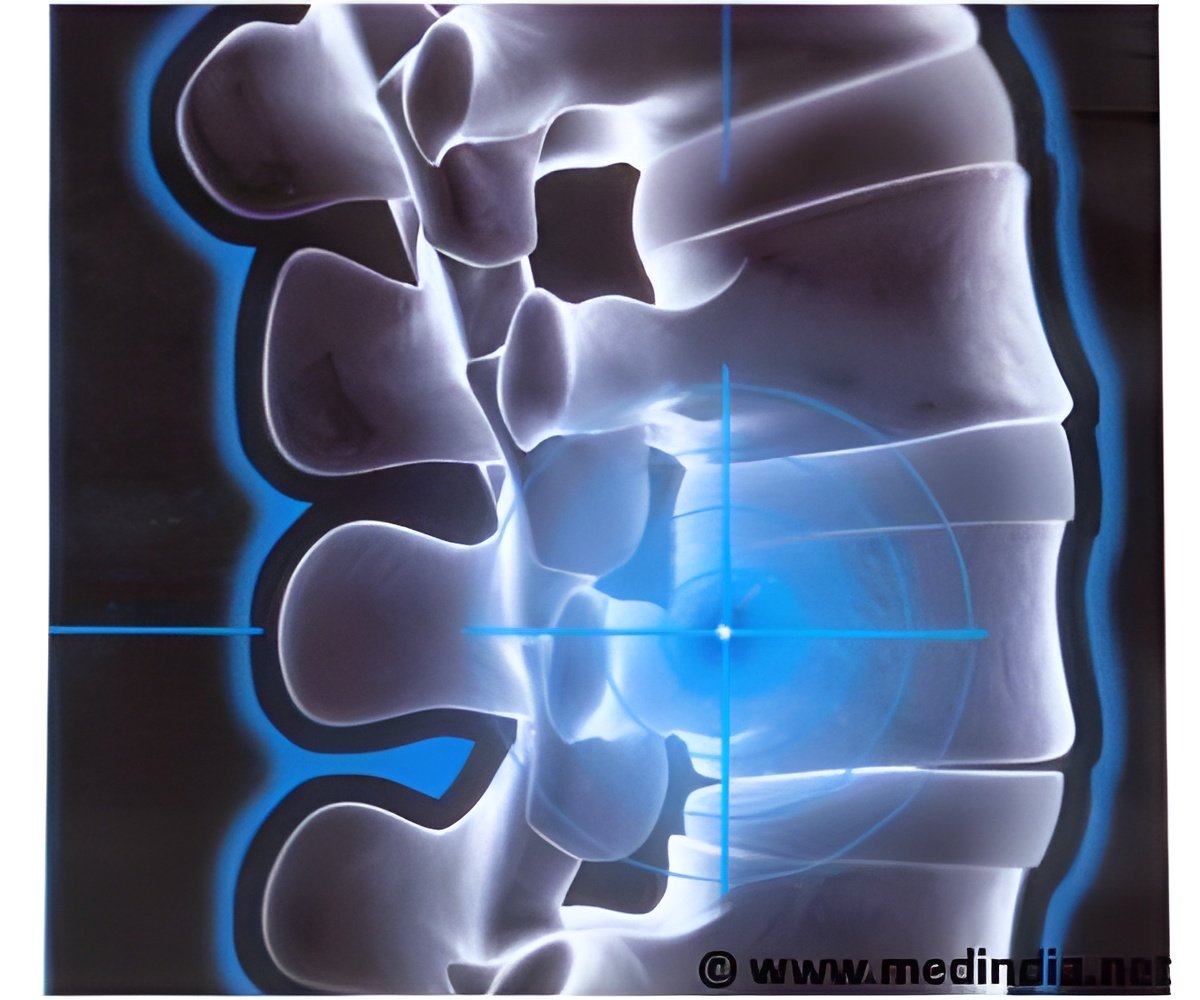
After 18 months, the researchers found that 82 percent of the RA participants were able to space out or stop their TNF-inhibitor injections without significant increases in either disease activity or functional impairment. However, the study did not demonstrate that the spacing approach was statistically equivalent to the traditional regimen. They also found that relapses occurred more frequently in the group that spaced injections compared to those who stayed on the same dosing schedule; but overall this did not result in differences in disease activity between the groups. The researchers are still analyzing X-rays to determine if the spacing strategy caused structural damage to their joints.
"A lot of effort has been dedicated to the development of new treatments for RA, leading to a substantial increase in RA costs. Nowadays, remission is achievable and treatment tapering needs to be considered and assessed," says Bruno Fautrel, MD, PhD, lead investigator in the study and professor at the University of Paris Medical Center in France. "RA is a chronic disease and the risk-benefit balance of taking DMARDs to manage the condition should be explored. Issues that should be evaluated include the risk of tapering or stopping DMARDs given that reducing medication may lead to flares and potential structural damage. Additional issues that should be considered are drug toxicity from continued DMARD use and substantial economic burden to society. This study explored the balance and tested the feasibility of biologic DMARD tapering (i.e., either interruption of current treatment or identification of the minimal effective dose)."
Source-Newswise













