Study sought to determine if lowering LDL cholesterol by inhibiting CETP had the same effect on the risk of CVD as other LDL cholesterol lowering therapies.

TOP INSIGHT
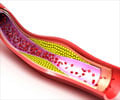
Cholesterol is naturally produced by your body and is essential to its function. However, excessively high levels of LDL cholesterol are bad and can lead to serious health problems such as clogged arteries, heart disease, and stroke.
"Therefore, the clinical benefit of LDL cholesterol lowering therapies may depend on the corresponding reduction in apoB particles, which in turn depend on how LDL cholesterol is lowered," he continued.
In the ACCELERATE trial, treatment with the cholesteryl ester transfer protein (CETP) inhibitor evacetrapib reduced LDL cholesterol by 39% (0.75 mmol/L) but did not reduce the risk of major cardiovascular events.2 The results led some people to question the causal effect of LDL cholesterol on the risk of developing CVD and suggested that the clinical benefit of lowering LDL cholesterol may depend on how it is lowered.
The current study sought to determine if lowering LDL cholesterol by inhibiting CETP had the same effect on the risk of CVD as other LDL cholesterol lowering therapies, and thereby determine if the clinical benefit of lowering LDL cholesterol depends on how LDL cholesterol is lowered.
The study included a total of 358 205 participants from 77 studies. The researchers used inherited genetic variants that mimic the effect of CETP inhibitors and statins, respectively, to naturally randomise participants into four groups: CETP inhibition (mimicking the effect of a CETP inhibitor), HMG-CoA reduction inhibition (mimicking the effect of a statin), both (mimicking the effect of combined CETP inhibitor and statin therapy) or neither (placebo group) using a 2x2 factorial Mendelian randomisation study design.
The investigators found that genetic variants that mimic the effect of CETP inhibitors were associated with higher high-density lipoprotein (HDL) cholesterol, lower LDL cholesterol, lower apoB and a corresponding lower risk of CVD that was proportional to the reduction in LDL cholesterol. In fact, genetic variants that mimic the effect of CETP inhibitors had a very similar effect on reducing the risk of cardiovascular events as genetic variants that mimic the effect of statins, ezetimibe and PCSK9 inhibitors when measured per unit reduction in LDL cholesterol.
The findings were validated in a genome-wide association study which found that other variants with discordant effects on LDL cholesterol and apoB were also associated with a lower risk of CVD that was proportional to the change in apoB but less than expected per unit change in LDL cholesterol.
Prof Ference said: "These results may help to explain the failure of some CETP inhibitors to reduce the risk of cardiovascular events despite robustly lowering LDL cholesterol. Adding a CETP inhibitor to a statin reduces LDL cholesterol out of proportion to apoB. Because the clinical benefit is determined by the reduction in apoB, rather than LDL cholesterol, combination therapy with a CETP inhibitor and a statin reduces the risk of cardiovascular events proportional to the attenuated reduction in apoB. This may be significantly less than expected for the observed change in LDL cholesterol depending on the degree of discordance between the reductions in apoB and LDL cholesterol."
Source-Eurekalert
 MEDINDIA
MEDINDIA




 Email
Email