Apart from treating cancer, base editing technique could help treat other conditions such as sickle cell disease.
Base-Edited CAR7 T Cells for Relapsed T-Cell Acute Lymphoblastic Leukemia
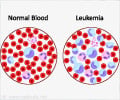
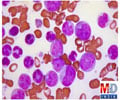
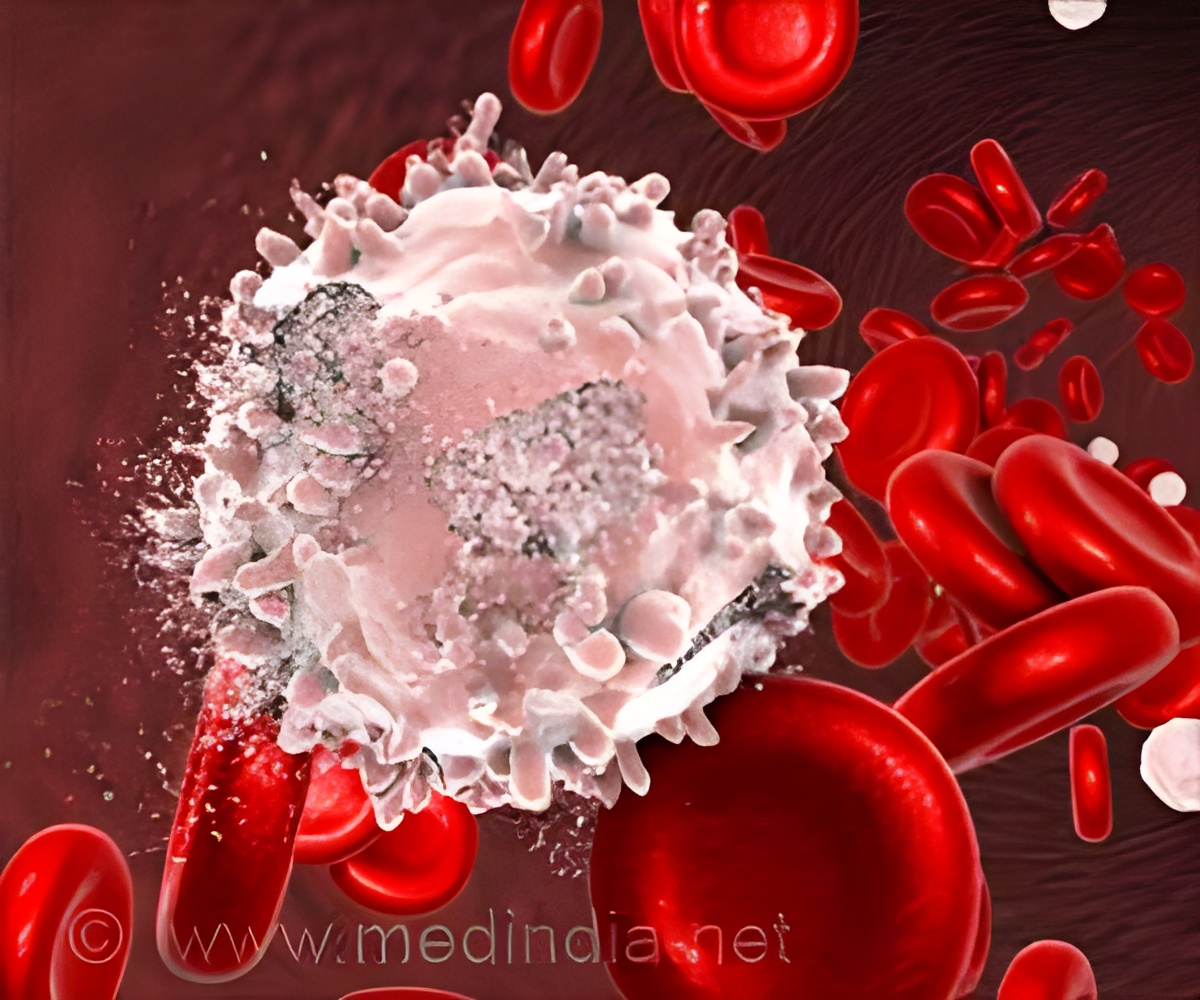
Go to source). The experience of using the cells in three patients is shared, and includes 13-year-old Alyssa from Leicester, who last year was //the first person in the world to be treated on the trial for T-cell acute lymphoblastic leukemia (T-ALL). This is a cancer of white blood cells and is usually treated with chemotherapy, but if it comes back, can be hard to clear.
Within four weeks of receiving the cells Alyssa’s leukemia was undetectable and she went on to have a successful bone marrow transplant, and is still well and at home almost a year later.
Is Base Editing Technology the Future of Leukemia Treatment?
A second teenager cleared their leukemic within a similar time period and is now recovering at home after their transplant. Sadly, while a third child responded to the CAR T cell therapy, their course was complicated by serious infections and their family agreed with the clinical team to move to palliative care.This first human application of base-editing technology was designed and developed by a team of researchers at UCL, led by Professor Waseem Qasim (UCL Great Ormond Street Institute of Child Health and Honorary Consultant at GOSH), working with Dr. Robert Chiesa and the Bone Marrow Transplant/CART/Hematology teams at GOSH.
The project is supported by the Wellcome Trust and National Institute of Health and Care Research (NIHR).
Professor Waseem Qasim, Professor of Cell and Gene Therapy at UCL, said: “It’s nice to be able to see the fruits of a long period of work coming together from multiple teams and being brought into play for new treatments. It’s still early, and we need more follow up and to treat more patients to know how it might impact treatments long term.”
Dr. Robert Chiesa said: “It is really crucial that children affected by cancer who failed standard of care have access to innovative strategies in the context of clinical trials such as this. A research hospital such as GOSH offers the ideal setting for developing experimental approaches that might offer hope to children with otherwise very poor prognosis. This is possible due to the dedication of scientists, doctors, nurses and allied professionals working for these children and their families.”
Advertisement
The steps were:
- Removing existing receptors so that T-cells from a donor can be banked and used without matching – making them ‘universal’.
- Removing a ‘flag’ called CD7 that identifies them as T-cells (CD7 T-cell marker). Without this step the T-cells – which are designed to recognise and attack cancerous cells – could also kill each other.
- Removing a second ‘flag’ called CD52. This makes the edited cells invisible to some of the strong drugs given to the patient during the treatment process.
Advertisement
The clinical trial for this treatment is still open and aims to recruit up to 10 NHS patients with T-cell leukemia, who have exhausted all conventional treatment options, referred by NHS children’s leukemia specialists. Patients are treated in the Bone Marrow Transplant Department at GOSH under the care of the BMT/CART/Hematology teams. Any patients eligible to receive treatment under the NHS and interested in this trial should approach their specialist healthcare provider.
If shown to be widely successful, the teams hope that it can be offered to more children and earlier in their treatment journey when they are less sick. With additional funding, they also hope to make it available for adults in the future.
Professor Qasim explained: “The technology itself could also have wide reaching applications for corrections of certain inherited conditions such as sickle cell disease. As the technology matures and is shown to be safe, it could be applied quite widely, although there will need to be careful testing and longer-term studies.”
The cells were manufactured as part of a long-standing research programme led by Professor Qasim at UCL Great Ormond Street Institute of Child Health. Thanks to early funding from Great Ormond Street Hospital Children’s Charity (GOSH Charity), Professor Qasim has been a pioneer in developing new CAR T-cell treatments using innovative gene editing techniques.
Reference:
- Base-Edited CAR7 T Cells for Relapsed T-Cell Acute Lymphoblastic Leukemia - (https://www.nejm.org/doi/full/10.1056/NEJMoa2300709)
Source-Eurekalert