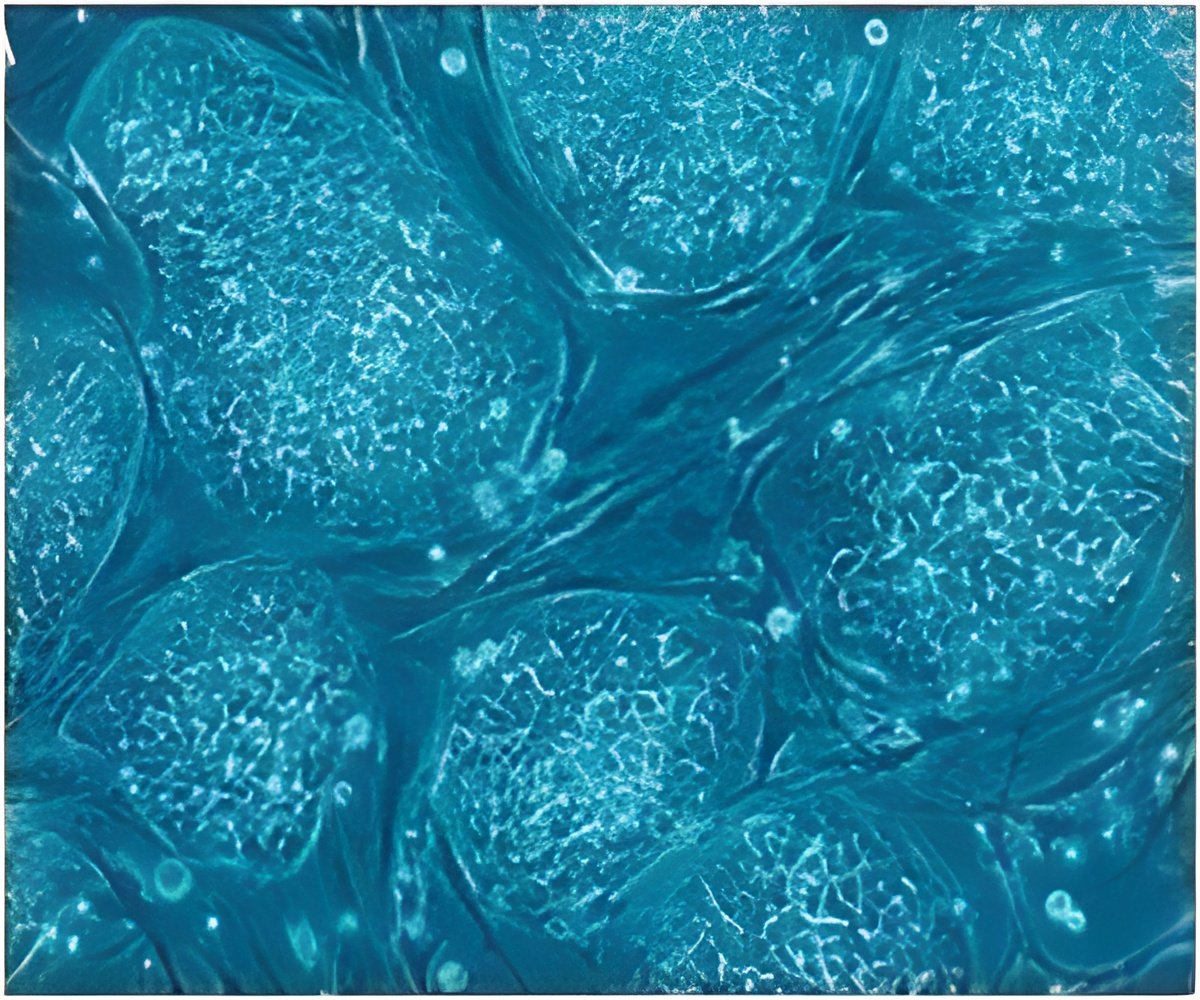
The micro-heart muscle that stretch into 3D tissue helps spur development and coaxes them to resemble as more mature cells making it easy for drug testing.
TOP INSIGHT
Heart cells created from skin-derived cells are challenging to make and work with, so creating large quantities can be difficult.
"In turn, this will enhance our ability to discover treatments for heart disease," Huebsch added.
Creating heart cells from induced pluripotent stem cells (iPSCs) that are derived from a patient's skin cells is inadequate for drug testing because they do not properly predict how a drug will affect adult heart cells.
Additionally, heart cells created from iPSCs are challenging to make and work with, so creating large quantities can be difficult.
The micro-heart muscle addresses these concerns. Forcing the cells to organise and stretch into 3D tissue helps spur development and coaxes them into resembling more mature cells that can better predict how a drug will affect adult heart cells.
Using fewer cells allows the scientists to do many more experiments with the same amount of resources.
"We think that the micro-heart muscle will provide a superior resource for conducting research and developing therapies for heart disease," he noted.
Source-IANS
 MEDINDIA
MEDINDIA


 Email
Email






