- 10 facts on guinea-worm disease - (https://www.who.int/dracunculiasis/epidemiology/en/)
- Dracunculiasis eradication - (www.who.int/features/factfiles/guinea_worm/en/)
What is Guinea-worm Disease (GWD)?
Guinea worm disease or dracunculiasis is an infection caused by the roundworm parasite Dracunculus medinensis. A parasite is an organism that either lives on or inside the body of another organism (the host) and survives by feeding off the host.
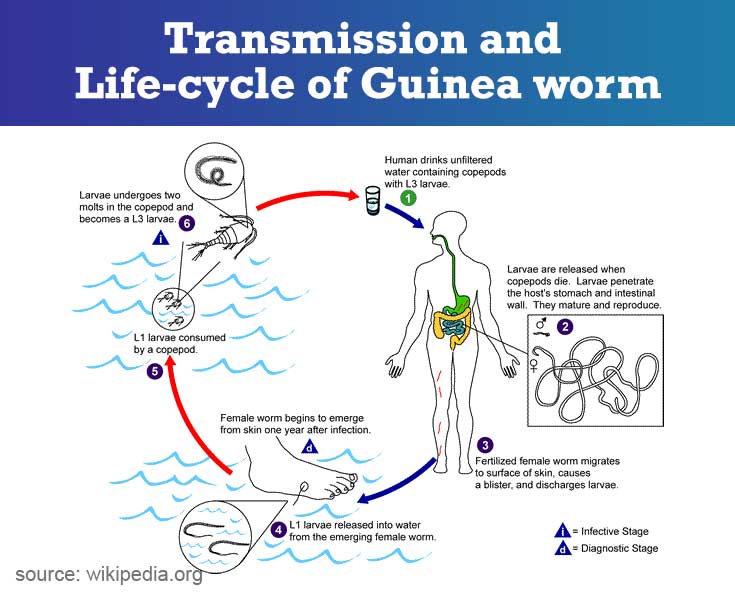
Guinea Worm Disease Spread
Guinea worm infection is transmitted when a person drinks contaminated water from ponds or wells that contain the immature form of the parasite (larva).
Guinea worm Disease - Epidemiology
- In 1986, there were about 3.5 million GWD cases reported annually in parts of Africa, Asia, and the Middle East.
- Thanks to the efforts of the Guinea Worm Eradication Program, only 30 cases were reported worldwide on 31st December 2017 from two countries namely Chad and Ethiopia
- In 2015 four countries were endemic for the disease namely Chad, Ethiopia, Mali and South Sudan
- Today the parasite has almost been completely eliminated.
Transmission and Life-cycle of Guinea worm
A person becomes infected by drinking water containing tiny infected crustaceans (hard-shelled animals that usually live in water). The immature guinea worms (larvae) live inside the crustaceans.
|
What are the Symptoms of Guinea-worm Disease?
- People remain asymptomatic until about one year after they have become infected (time taken for larvae to develop into adults and migrate from the abdominal cavity).
- Guinea worm disease symptoms start when the worm tries to break out through the skin
- A few hours to days before the worm emerges from the skin blister, the person may develop pain and swelling in the area associated with fever in the area.
- Occasionally proteins released by the worm can cause an allergic reaction, leading to breathing difficulty, an itchy rash, vomiting and disabling pain.
- Nearly all the worms come out through the legs and feet, but they can come out through other parts as well
- Usually, the blister heals spontaneously once the adult worm leaves the body. However, in some people, superadded bacterial infections develop around the blister
- Sometimes joints and tendons adjacent the blister are affected, causing joint pain and inflammation and features of arthritis
How to Diagnose Guinea-worm Disease?
Diagnosis of guinea worm disease is usually made by clinical examination of patient while the adult worm is protruding from a skin blister
- In suspected cases – particularly in endemic areas with persons having painful blister or sore on the lower limb
- Confirmation on examination of lesion with Guinea worm protruding out through the blister. These adult worms measure 60-100 centimeters (2-3 feet) long and as wide as a cooked spaghetti noodle.
If skin blister has healed and there are no active lesions, x-rays of the limbs may reveal calcified nodules beneath the skin especially in endemic areas.
How to Treat Guinea-worm Disease?
- There is no drug to treat dracunculiasis and no vaccine to prevent the disease.
- The only treatment is to remove the worm by winding it around small stick and pulling it out one little bit at a time as it loosens. Sometimes the worm can be pulled out completely within a few days, but it may take upto several weeks or months.
- If health care personnel are available, the worm can be removed through a small incision made in the area after injecting a local anesthetic
- Sometimes the worm can be surgically removed by a trained surgeon before formation of the blister
- Analgesics, such as aspirin or ibuprofen may be given to decrease pain and swelling. Topical antibiotic creams can help development of secondary bacterial infections
How to Prevent Guinea-worm Disease?
- Drink water only from protected water bodies free of contamination, such as bore wells or hand-dug wells with a wall around the sides and covered at the top
- Restrict persons with sores, blisters, wounds and hanging Guinea worms from entering these ponds or other water sources
- Water from unsafe sources should always be filtered using a cloth filter or a pipe filter, to remove the crustaceans (copepods) that cannot be seen by the naked eye
- Unsafe drinking water sources should be chemically treated with an approved larvicide, such as ABATE®*. This will kill the copepods that contain Guinea worm larvae.
- Ensure provision of persons living in endemic communities with safe drinking water
- Teaching villagers to cook their fish properly, and to bury tissue left over from processing of the fish, and to not allow their dogs to eat this tissue or uncooked fish
- Encourage dog owners to keep out infected dogs until the worms come out and to prevent them from contaminating drinking water
Guinea-worm Global Eradication Program - WHO Facts and Figures
- In 1981, the steering committee of the International Drinking Water Supply and Sanitation Decade (1981–1990) proposed the elimination of dracunculiasis as an indicator of success of the decade
- The World Health Organization (WHO) endorsed the above suggestion in the same year
- Following this the WHO and the US Centers for Disease Control (CDC) formulated a strategy and drew up guidelines for this eradication campaign
- The Carter Center joined the movement in 1986 and has been in the thick of action since then in partnership with the WHO and UNICEF
- In 1995, an independent International Commission for the Certification of Dracunculiasis Eradication (ICCDE) was established by the WHO
- In 2011 the WHO called upon its member states to work for the eradication of dracunculiasis by making coordinated efforts to reduce transmission
The success of the program is readily evident from the following figures and data
- In 1986 3.5 million new cases were reported from nearly 20 countries
- Since the inception of the program, the number of countries reporting new cases has been gradually decreasing and in December 2017 only Chad and Ethiopia reported 30 cases between themselves.
- Several countries in Africa, the Middle East and Asia have successfully eradicated the disease during this period
- Disease surveillance in endemic countries is done by health workers and in countries where transmission has been interrupted, a further three year period of surveillance is maintained to ensure complete eradication
- Thousands of village volunteers in the remaining endemic countries are trained to detect new cases, attend to them, educate them and their families on preventive measures. The new cases are reported to the area supervisor
- Since its founding in 1995 until April 2016, the ICCDE has convened 11 times and certified 198 countries, territories and areas to be Guinea worm free; the latest nation to achieve this distinction was Ghana in 2015, a formerly endemic country
- To declare global elimination of Guinea worm disease, WHO must formally certify every single nation even if the disease or its transmission has never been recorded in that country.