- Erysipelas and cellulitis: Overview - (https://www.ncbi.nlm.nih.gov/books/nbk303996/)
- Cellulitis and Erysipelas - (http://www.bad.org.uk/shared/get-file.ashx?id=156&itemtype=document)
- What are erysipelas and cellulitis? - (https://medlineplus.gov/ency/article/000618.htm)
- Erysipelas - (http://www.ifd.org/protocols/erysipelas-and-cellulitis)
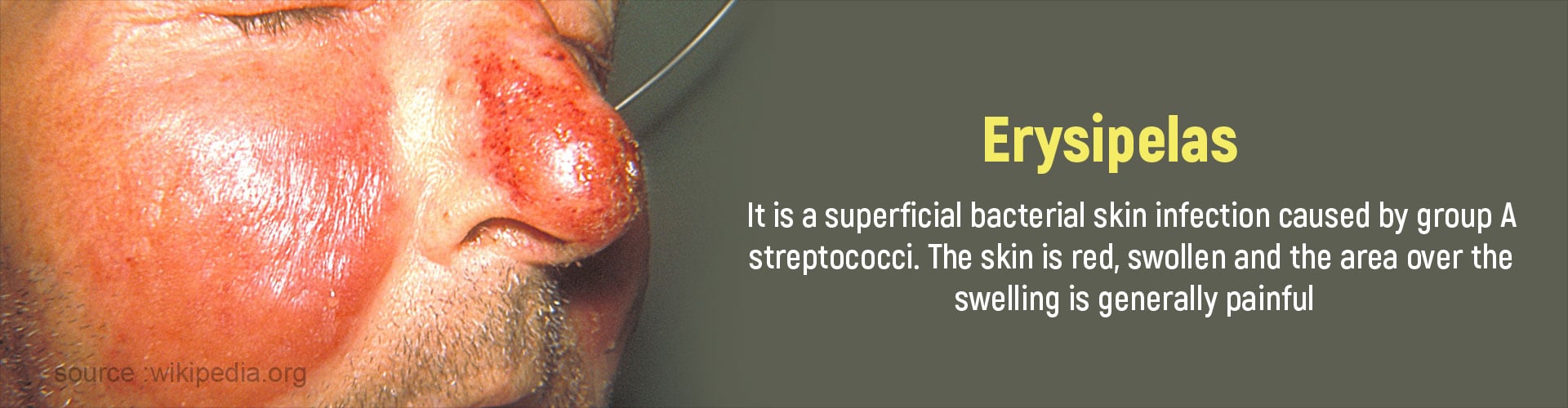
What is Erysipelas?
Erysipelas is a bacterial infection of the superficial layers of the skin Bacteria enter the skin through sores and cuts causing the skin to become swollen and red. Usually the outer layer (epidermis) of the skin and the associated lymph nodes are infected.
It is similar to and is considered to be a variant of another form of skin infection called cellulitis which affects the deeper layers of the skin and subcutaneous tissues.
The skin of fingers, toes, arms, lower legs, and face, the skin surrounding the eyelids, cheeks, and the skin of the belly are invariably affected in erysipelas. Erysipelas is commonly observed in tropical countries
Young children and elderly persons with a weak immune system are particularly susceptible to develop erysipelas.
What are the Causes and Risk Factors of Erysipelas?
The bacteria beta-hemolytic streptococci (BHS), especially group A streptococci (mainly Streptococci pyogenes) are usually responsible for causing erysipelas. Staphylococci may also be involved in causing infections though their role is still uncertain.
Some of the risk factors of erysipelas are as follows:
- Skin rash
- Underlying eczema
- Animal or insect bites
- Fungal infections e.g. Athlete’s foot (This infection often gives rise to secondary bacterial infection that may cause recurrent erysipelas
- Injuries on the skin
- Circulation problems eg. varicose veins
- Surgical wounds
- Weak immune system especially children and elderly persons
- Pinpricks
- Cancer
- Congenital lymphedema
- Intravenous use of drugs
- Alcoholism
- Obesity
- Drugs used to treat psoriasis that suppress immunity

What are the Signs and Symptoms of Erysipelas?
Erysipelas is characterized by the following symptoms that develop quickly from a few hours to a few days
- The affected area becomes raised (plaque) and appears bright red in Caucasians and brownish-grey in dark-skinned individuals.
- There may be blisters on the affected area filled with clear fluid or blood. There is marked tenderness and pain over the affected area.
- Chills, nausea, and sudden onset of high fever precede the changes on the skin.
- The surface of the plaque is shiny, raised with well-defined borders. It feels hot to touch and spreads rapidly across the skin if untreated.
- Local lymph glands may be swollen and tender.
How do you Diagnose Erysipelas?
Erysipelas is diagnosed primarily by clinical symptoms and typical findings on physical examination. It is treated with mild or long-term antibiotics depending on the stage of infection.
A skin biopsy is generally not performed since skin cultures may not give conclusive results.
Any recent injury in your medical history can give a clue to the condition. If a wound is caused by an animal bite, the fluid from the wound may be tested for bacteria.
What are the Complications of Erysipelas?
Erysipelas can cause the following complications if the infection is severe or left untreated.
- Lymphedema: Bacterial infection may destroy some parts of the lymphatic system. This causes lymph to build up in the body Lymphedema is a major risk factor for the recurrence of erysipelas
- There may be localised collections of pus filled cavities on the skin (abscess)
- Bacteremia: The bacteria may travel to the blood and affect the joints, heart valves, and bones.
- Septicemia: Blood poisoning can occur due to bacterial infections.
- Meningitis: Facial erysipelas may cause meningitis
- Recurrent erysipelas may occur at the same site of initial infection
- Death of affected tissue resulting in gangrene
- Kidney damage may occur
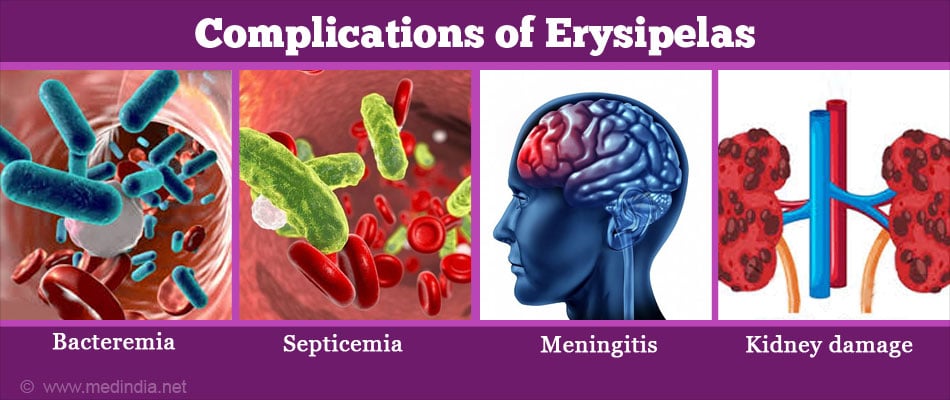
Although rare, if these complications occur, it is advisable that they are treated immediately to avoid further damage.
Abscess and meningitis are complications more likely to develop where the bacterial infections spreads to the deeper layers of the skin (cellulitis).
How do you Treat Erysipelas?
Medications
Erysipelas is treated with mild, oral antibiotics for one to 2 weeks. Recurrent erysipelas is treated with long-term antibiotics. Intravenous penicillin G and flucloxacillin in high doses are effective in treating erysipelas. Macrolides and amoxicillin are the other recommended antibiotics.

If fungal infection (athlete’s foot) is the cause of erysipelas, antifungals are given Painkillers are administered to reduce the pain.
Anticoagulants (medications that prevent blood clotting) are administered to those at risk of venous thromboembolism. It is advisable to be mobile and to drink plenty of fluids to avoid dehydration.
Supportive Measures
Erysipelas of the leg is treated by placing the leg in an elevated (higher than the hip) position during bedrest. The gravity helps to reduce the swelling.
Surgery
In severe cases when there is extensive damage to the skin and death of tissue, surgery is necessary to remove the dead tissue. Fortunately this is very rare nowadays.
How do you Prevent Erysipelas?
- Since erysipelas occurs due to cracks in the skin, it is advisable to take good care of your skin by regular cleaning. Use of antiseptics (topical creams) or moisturizers is preferred in such cases.
- Always keep wounds clean and dry
- Avoid scratching the affected area if you have any skin condition
- Treat any skin problems such as eczema or athletes foot promptly
Health Tips
Keeping the leg elevated, losing weight, and use of support stockings can all help in managing the swelling due to leg erysipelas.
Skin should be taken care of in order to prevent any cuts or sores and hence avoid infection.
 MEDINDIA
MEDINDIA
 Email
Email





