Children suffering from a rare Hurler's syndrome can now be treated more effectively using stem cells from the umbilical cord as opposed to the previous transplant of matched donor stem cells.

"Cord blood has been proposed as an alternative stem cell source for children with HS since it has been suggested that cord blood may increase their levels of lysosomal α-L-iduronidase, which consequently may allow them to live longer with fewer complications," said lead study author Jaap Jan Boelens, MD, PhD, of the University Medical Center Utrecht, in Utrecht, Netherlands. "However, until now, no studies have compared the safety and efficacy of different stem cell and donor sources among a large group of patients to determine which may be the ideal transplant source."
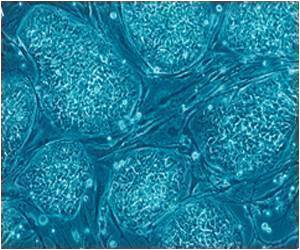
With this aim, Dr. Boelens and a team of investigators conducted a retrospective analysis analyzing outcomes of HS patients treated with HCT in centers affiliated with the European Group for Blood and Marrow Transplantation (EBMT), Eurocord, and the Center for International Blood and Marrow Transplant Research (CIBMTR). A total of 258 infants and children with HS (ranging from 2 months to 18 years, with a median age of 16 months at transplant) who received an HCT between 1995 and 2007 were selected for analysis based upon certain criteria: a confirmed diagnosis of HS; a transplant of cells from a matched sibling donor (MSD), a matched or mismatched unrelated donor (UD), or cells from a single, unrelated cord blood (UCB) unit; and pre-transplant treatment containing a high dose of chemotherapy to help prevent their immune systems from rejecting donated cells.
Nearly half of the children evaluated in the study (45%) had received transplants of unrelated cord blood (81% of which was from mismatched donors) with the others receiving transplants of bone marrow stem cells from unrelated donors or matched sibling donors. All the patients received pre-transplant high-dose chemotherapy, and 19 percent had previously received intravenous enzyme replacement therapy with lysosomal α-L-iduronidase. Taking into consideration stem cell source and pre-transplant conditioning, the team compared the rates of overall survival (OS), event-free survival (EFS), engraftment (the degree to which transplanted donor cells were able to reproduce into new cells) or graft failure, or death.
The team noted encouraging survival rates among the children with HS who had received an HCT, regardless of source, with 5-year estimated OS and EFS at 74 percent and 63 percent, respectively. Importantly, EFS rates were similarly high for children who had received donations of matched sibling cells or fully matched unrelated umbilical cord blood (MSD or UCB, 81%), compared to EFS rates for patients transplanted with cells from matched unrelated donors (66%) or unmatched unrelated cord blood donors (68%). EFS rates were highest among infants who received transplants at age 16 months or younger, indicating the importance of transplantation as early as possible after diagnosis for these children, when treatment may help prevent further disease burden or damage.
Within two months of undergoing transplants, nearly all patients (91%) showed evidence of donor cell recovery (as noted by increasing levels of white blood cells in the blood). Only 12 percent of children experienced secondary graft failure (when the body rejects donor cells).
After completing their analysis of the children, whose progress had been tracked for approximately five years post transplant, Dr. Boelens' team concluded that the children who received UCB transplants experienced on average a higher rate of donor cell engraftment (complete replacement of the bone marrow by donor cells) and normal enzyme levels than those who had received transplants of matched sibling cells or matched/unmatched unrelated bone marrow stem cells. Nearly all (98%) of the cord blood recipients whose transplanted cells were successfully engrafted had normal enzyme levels, supporting a link between high levels of lysosomal α-L-iduronidase in cord blood and suggested improvements in long-term outcomes among HS patients who receive UCB transplants.
 MEDINDIA
MEDINDIA



 Email
Email








