‘A brain protein – YKL-40 that is regulated by clock genes is also involved in clearing away the toxic buildup of Alzheimer's protein plaques in the brain. This sheds light upon YKL-40 as a possible link between circadian rhythm dysfunction and Alzheimer's, and therapies targeting the protein may slow the course of the disease.’
Tweet it Now
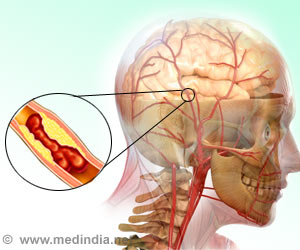
It was also found that Alzheimer's patients who carry a genetic variant that reduces YKL-40 levels maintain their cognitive faculties longer than people without the variant. Alzheimer’s disease (AD) is a neurodegenerative disease that leads to gradual memory loss and behavioral changes. It is characterized by the formation of beta-amyloid plaques and the tau proteins in the brain tissues, long before the actual symptoms occur.
The circadian rhythm is a natural, internal master clock in the brain that regulates our daily rhythms of the sleep-wake cycle. This cycle also regulates the various body functions – sugar absorption to body temperature to immune and inflammatory responses.
"If your circadian clock is not quite right for years and years -- you routinely suffer from disrupted sleep at night and napping during the day -- the cumulative effect of chronic dysregulation could influence inflammatory pathways such that you accumulate more amyloid plaques. We hope that a better understanding of how the circadian clock affects YKL-40 could lead to a new strategy for reducing amyloid in the brain", says the senior author Erik Musiek, MD, Ph.D., an associate professor of neurology.
Sleep Biomarkers in Alzheimer’s Disease:
Advertisement
"If you have inflammation in the morning, you might get lots of YKL-40; if you get inflammation in the evening when the clock's in a different phase, you might get less YKL-40," says Musiek.
Advertisement
Amyloid plaques normally are surrounded by immune cells called microglia that help keep the plaques from spreading. In the mice that lacked YKL-40, the microglia were more plentiful and more primed to consume and remove amyloid.
The findings were supported by research on 778 people who participated in aging and dementia studies at the university's Charles F. and Joanne Knight Alzheimer's Disease Research Center. Approximately a quarter (26%) of them carried a genetic variant that reduces levels of YKL-40. Cognitive skills declined 16% more slowly in the people with the variant.
"People have been measuring YKL-40 in spinal fluid for several years, but we were never sure of its function if it was good or bad. Our data suggest that in Alzheimer's, it's bad. People who have less of it fare better. If you could design a therapy to lower YKL-40, it might help the microglia remove more amyloid and maybe slow the progression of the disease", says Musiek.
Thus, the study sheds light upon YKL-40 as a possible link between circadian rhythm dysfunction and Alzheimer's, and that therapies targeting the protein may slow the course of the disease.
Source-Medindia