Potentially safer and more effective gene therapy vector for blood disorders have been developed.
‘Potentially safer and more effective gene therapy vectors for blood disorders like sickle cell disease and beta-thalassemia have been developed. The newly engineered vector is designed to overcome the side effects of conventional gene therapy, which in turn improves the curative therapy for various blood disorders.’





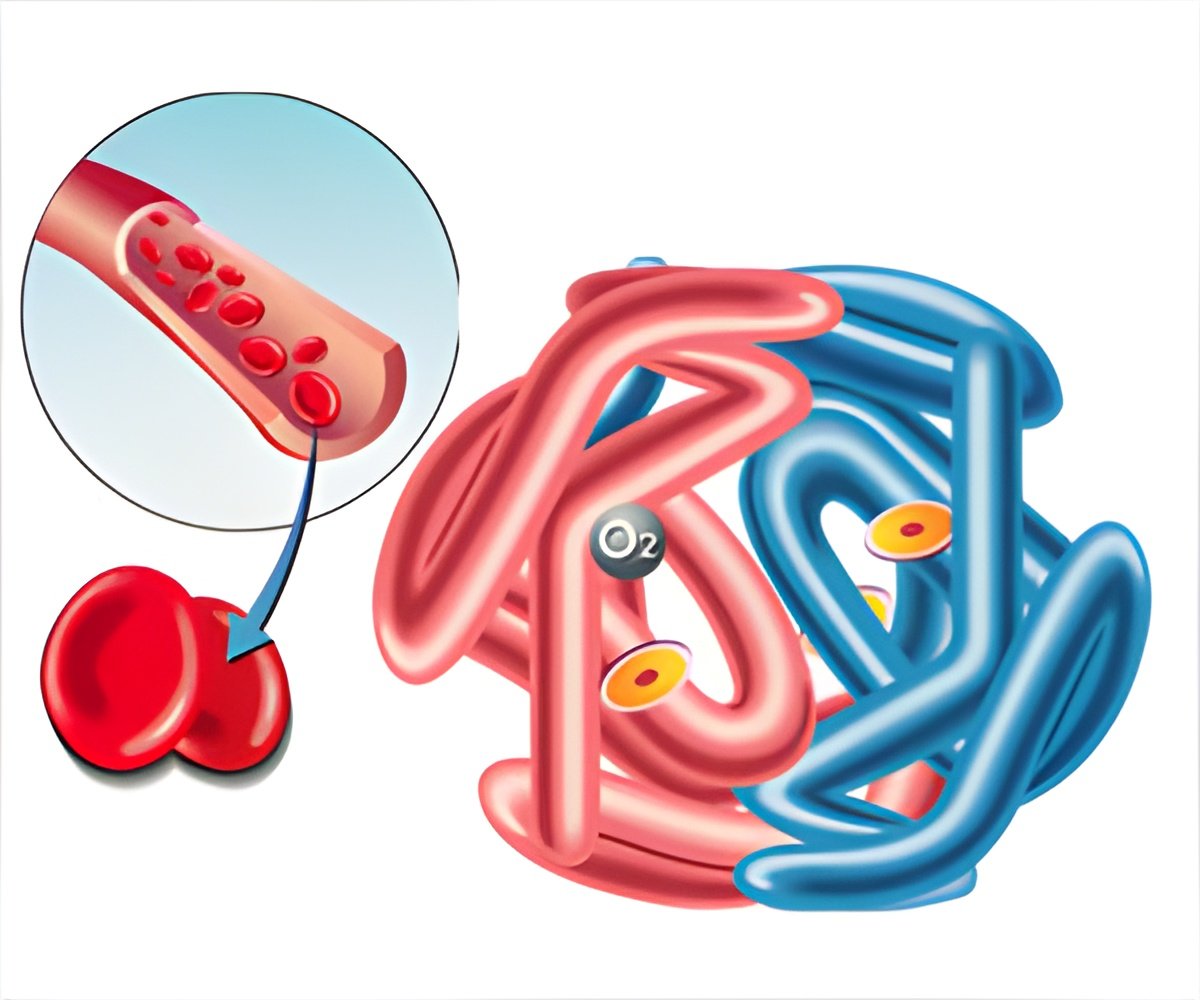
The vector is a designed carrier vehicle that delivers functional copies of the hemoglobin gene to rectify a genetic abnormality and restore normal hemoglobin production in patients. Prompt creation of more hemoglobin with a lower dose, limits the risk of toxic side effects. "These results have many potential benefits for the successful treatment of patients affected by beta-globinopathies like sickle cell disease and beta-thalassemia, including a better dose-response, a minimized chance of clonal expansion and tumorigenesis, a reduced cost of therapy, and a potentially reduced need for chemotherapy or radiation before beginning gene therapy", says Laura Breda, Ph.D., research assistant professor at CHOP and first author of the paper.
Sickle cell disease and beta-thalassemia also known as beta-globinopathies, are a type of genetic blood disorders that are known to be caused by errors in the genes for hemoglobin. It occurs due to the mutations in the beta-globin gene that may lead to serious health complications, ranging from delayed growth and jaundice to pain crises, pulmonary hypertension, and stroke.
Engineered Gene Therapy
Conventional gene therapy is said to hold many challenges like limited dose-response, dose-related toxicities, and the need for myeloablation in many cases – a procedure in which the bone marrow is suppressed via chemotherapy or radiation before gene therapy can begin.
Advertisement
Lentivirus – the same retrovirus used to create conventional gene therapy vectors for beta-globinopathies, is utilized by re-engineering it.
Advertisement
With the aid of multiple in vitro and in vivo screening methodologies, one of their newly designed vectors, ALS20, was seen to express a higher level of transgenic hemoglobin as compared to other vectors that are currently in use to treat beta-globinopathies.
ALS20 is said to produce 157%, 84%, and 40% more adult hemoglobin, as compared to the three benchmark vectors. This would be beneficial to those patients who require higher hemoglobin production to become transfusion independent.
"Considering the body of evidence presented in this work, we believe that ALS20 is an outstanding candidate for the successful treatment of beta-globinopathies. Our vector may not only provide safer therapy with a reduced probability of genome toxicity and milder conditioning requirements, but it may also improve the efficacy and offer a competitive product for the gene therapy market", says senior author Stefano Rivella, Ph.D., Kwame Ohene-Frempong Chair on Sickle Cell Anemia and Professor of Pediatrics at CHOP.
This improved curative therapy for blood disorders is being further explored to move the newly designed vector into clinical trials.
Source-Medindia