Higher follow-up rates with pulmonologist post hospitalization in advance practice provider (APP) group may partly explain the lower trends in emergency visits.
TOP INSIGHT
The University of Texas Medical Branch's study is the first to examine the quality of COPD primary care delivered by physicians versus APPs on a national level.
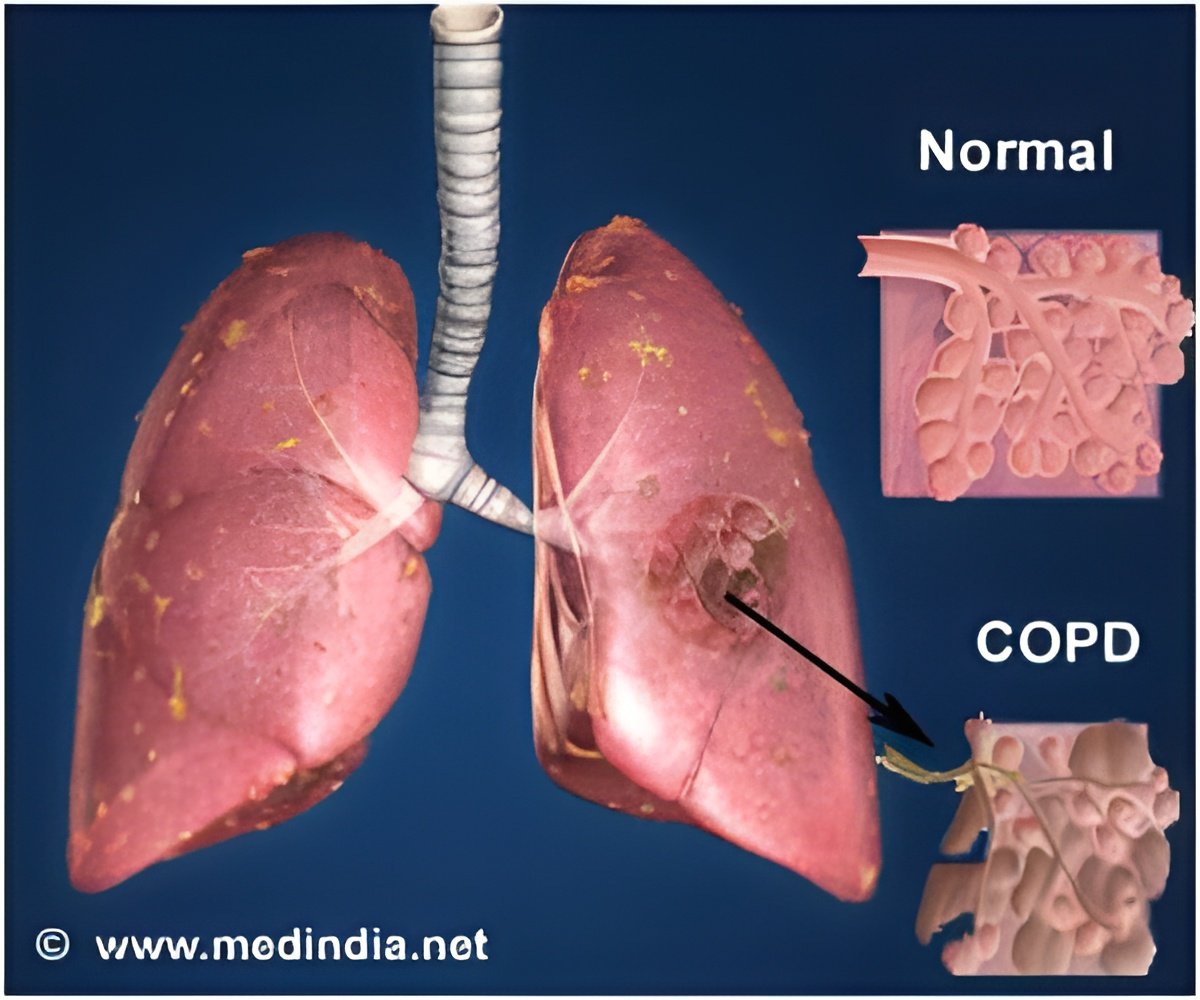
APPs are increasingly contributing to the care of those with health conditions requiring lifelong management such as chronic obstructive pulmonary disease, diabetes, high blood pressure and others. However, some physician organizations say that APPs have less training and experience managing these type of conditions and can't deliver services of as high quality or as safe as those of physicians.
UTMB's study is the first to examine the quality of COPD primary care delivered by physicians versus APPs on a national level. For the study, records of 7,257 Medicare COPD patients who had at least one hospitalization in 2010 were reviewed. Researchers were looking for differences in the medical care given by the two types of providers and outcomes of patients.
The researchers looked at which health care professionals administered tests to check breathing capacity, flu and pneumonia vaccines, COPD medications and referrals to a pulmonary specialist. Outcome measures were emergency department visits, number of hospitalizations and readmissions within the first month after being released from the hospital.
"We found that APPs were more likely to prescribe short-acting inhalers or oxygen therapy and to consult with a pulmonary specialist, but less likely to give flu and pneumonia vaccinations compared to physicians," said Amitesh Agarwal, MD, lead author and fellow in the UTMB division of pulmonary critical care & sleep medicine. "Patients receiving care from APPs had lower rates of ER visits for COPD and a higher follow-up rate with a pulmonologist within 30 days of hospitalization for COPD than those cared for by a physician."
The study also found lower rates of follow-up clinic visits after hospitalization for sudden COPD flare-ups in the APP group than in the primary care physician group. However, patients cared for by APPs had more clinic follow-up visits with a pulmonary specialist than the patients of physicians. Higher follow-up rates with pulmonologist post hospitalization in APP group may partly explain the lower trends in emergency visits and readmission.
 MEDINDIA
MEDINDIA


 Email
Email










