A team of scientists, led by researchers at The Wistar Institute, has found that an infection with herpes simplex virus 1 (HSV-1) causes rearrangements in telomeres.
"We know that telomeres play a very important part in the lifespan of a cell," said Paul M. Lieberman, Ph.D., Hilary Koprowski, M.D., Endowed Professor and Professor and Program Leader of the Gene Expression and Regulation Program at The Wistar Institute. "We wanted to know whether they also play a role in either viral replication or protection from viruses, and our findings suggest - at least in the case of the herpes simplex virus - that this may indeed be the case."
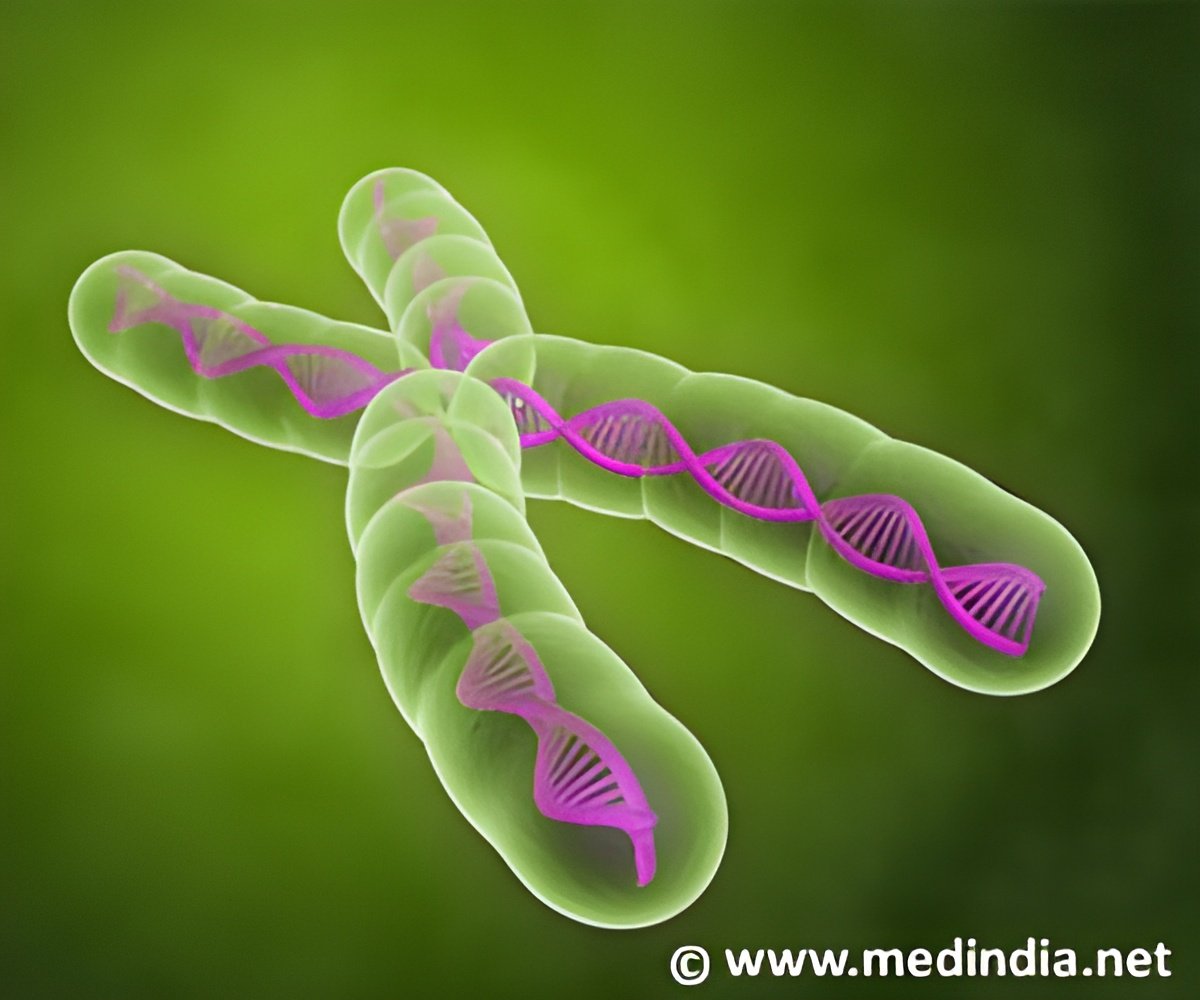
Telomeres are often compared to the clear tips of shoelaces because they protect the end of chromosomes - the keepers of our vital genetic information - and prevent them from fraying and breaking, thus preserving their ability to pass on necessary genetic information. Previously, Lieberman's lab at Wistar has shown that viral DNA replication and maintenance share some common features with telomeres.
"Telomeres may serve as a barrier to viral replication," Lieberman said. "We wanted to explore whether that protection was at a physical level or a more molecular level."
Among the viruses Lieberman and his lab have decided to study is HSV-1, a particularly aggressive virus that replicates in the nucleus of a healthy cell where chromosomes and their telomeres reside. HSV-1 is a common virus that causes cold sores but can also cause more serious diseases including blindness and encephalitis. In the United States, approximately 65 percent of the population has antibodies to this particular strain of the virus as well as latent infections that can periodically reactivate to cause clinical symptoms. There is no vaccine for preventing HSV-1 infection and reactivation, and only a few effective treatments for the virus are available.
As detailed in the study, the Lieberman lab found that HSV-1 is able to induce the transcription of telomere repeat-containing RNA (TERRA). This is followed by the virus degrading a telomere protein called TPP1 - part of a complex of proteins responsible for protection called "telomere sheltering" - which results in the loss of the telomere repeat DNA signal. When TPP1 becomes inhibited, the virus is able to increase its ability to replicate, suggesting that TPP1 normally provides some sort of protective function against this virus. HSV-1 is able to replicate more efficiently by disabling this protection. Finally, the virus uses a replication protein called ICP8 that works with the manipulated telomeric proteins to promote viral genomic replication.
Advertisement
Advertisement