Ischemia‐ and inflammation‐induced human proliferative diabetic retinopathy microenvironment supports pathological neolymphvascularization, bringing a new concept to the proliferative diabetic retinopathy mechanisms and targeting options.
- Eye complication in diabetes may contribute to lymphatic neovascularization.
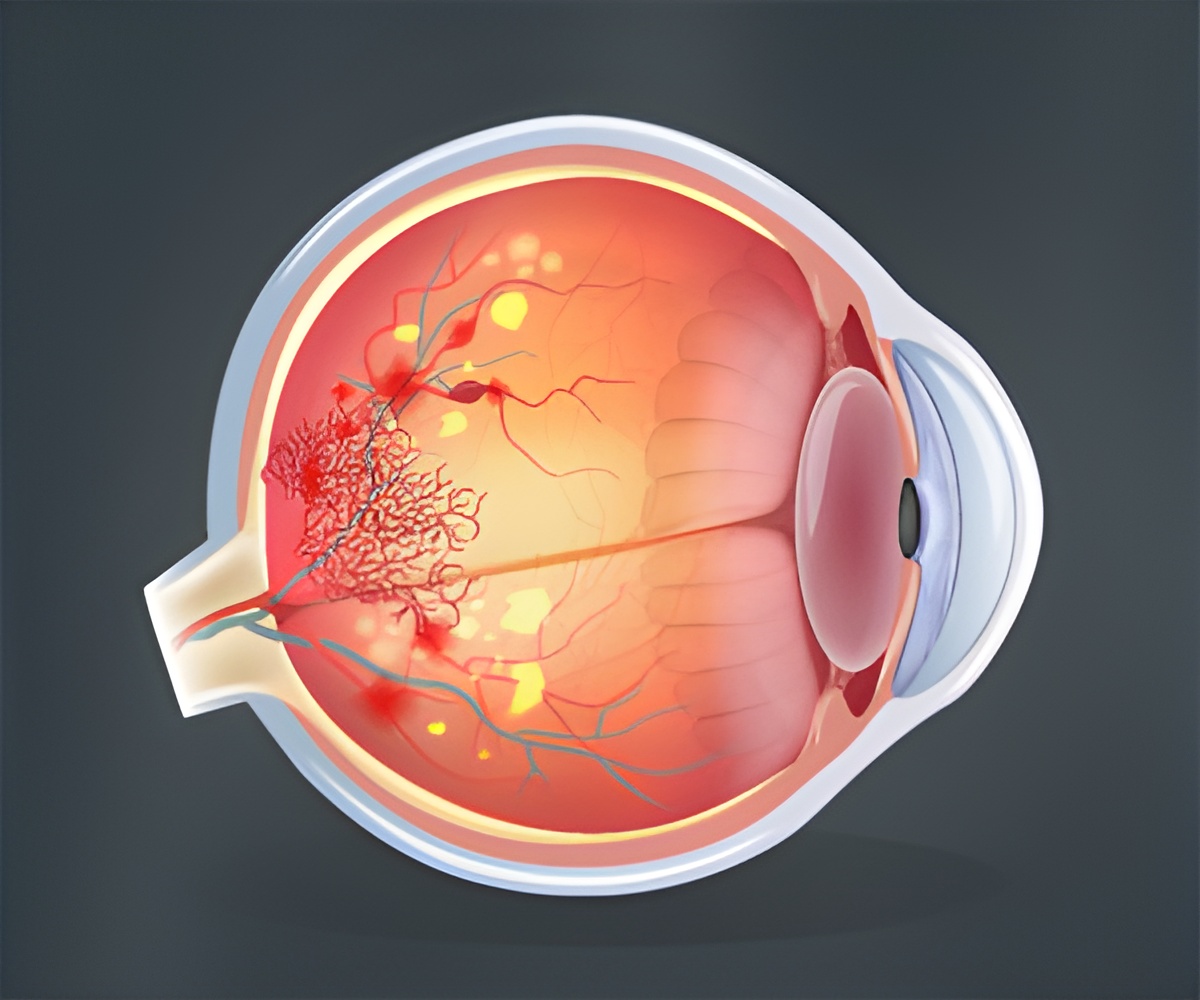
- This eye complication is called proliferative diabetic retinopathy.
- It is a major sight-threatening diabetic complication.
A major sight-threatening diabetic complication called proliferative diabetic retinopathy is developed by more than 60 percent of diabetes patients 20 years after diagnosis with diabetes despite metabolic control, research at the University Of Helsinki finds. Proliferative diabetic retinopathy occurs when endothelial cells of the retinal vasculature invade their surroundings and project into the vitreous, the gel substance present inside the eye. Weakness in the new vessels leads to vitreous hemorrhage and a fibrotic response that will eventually pull the retina causing retinal detachment and subsequent vision loss. When these vessels develop, diabetic patients are directed to vitreoretinal surgery whereby the newly formed pathological fibrovascular tissue is excised.
TOP INSIGHT
The microenvironment of proliferative diabetic retinopathy may be a supportive environment for the development of pathological neolymphvascularization. This finding may help identify a novel target for diabetic retinopathy therapy.
The challenge was to understand the nature of these vessels.
Chronic tissue inflammation is present in proliferative diabetic retinopathy is connected with lymphangiogenesis. Therefore the research team investigated whether proliferative diabetic retinopathy involves the growth or differentiation of new lymphatic vessels.
An expression of lymphatic markers in the proliferative diabetic retinopathy tissues was found.
Knowing the microenvironment is of fundamental importance to understand the mechanisms of a disease. The close collaboration between clinics and research laboratory opened such avenue, says Research Director Kaisa Lehti, Karolinska Institutet and University of Helsinki.
Applications of research findings
The functionality of these vessels in PDR pathogenesis remains to be investigated. It is important to know whether these lymphatic vessels develop coincidentally with abnormal blood vessels or only later upon PDR progression and whether they are detrimental or beneficial.
Future therapeutic strategies targeting both lymphangiogenesis and angiogenesis may represent promising approaches for treating ischemia and inflammation-associated posterior segment retinal diseases, states ophthalmic surgeon, Dr. Sirpa Loukovaara from Helsinki University Hospital.
References:
- Erika Gucciardo, Sirpa Loukovaara et al. Microenvironment of Proliferative Diabetic Retinopathy Supports Lymphatic Neovascularization, The Journal of Pathology https://doi.org/10.1002/path.5070
Source-Medindia
 MEDINDIA
MEDINDIA



 Email
Email










