Cyclophosphamide or MMF with a corticosteroid is the first treatment choice for lupus nephritis. On the other hand, azathioprine or MMF combined with a corticosteroid is useful as maintenance therapy.
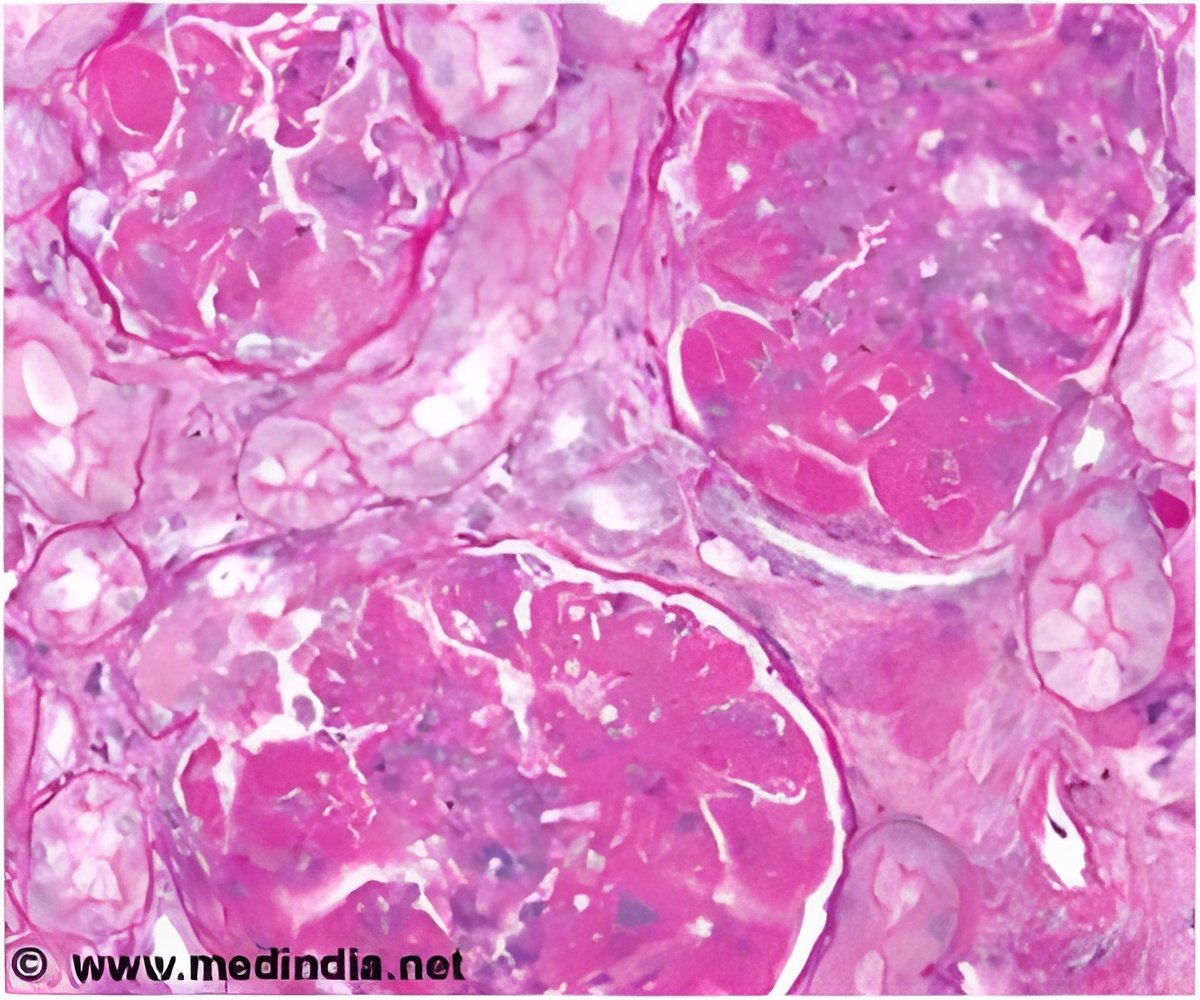
The American College of Rheumatology (ACR) describes lupus nephritis as continuous proteinuria (protein in urine) of more than 0.5 g/day and/or urinary casts. Urinary casts are cylindrical structures produced by the kidney in disease states. A kidney biopsy is required to diagnose lupus nephritis.
The International Society of Nephrology and the Renal Pathology Society (ISN/RPS) modified World Health Organization (WHO) classification of lupus nephritis into 6 classes as per the seriousness and degree of disease.
Treatment goals include improvement in kidney function and delay in kidney failure. An angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) is suggested for patient with proteinuria ≥0.5 g/day (ISN/RPS class I-II). On the other hand, ISN/RPS classes III-IV lupus nephritis patients need to be treated with immunosuppressive drugs (drugs that suppress immunity).
Antimalarials, such as hydroxychloroquine, are recommended for all SLE patients with nephritis since they effectively decrease disease progression and promote recovery.
Cyclophosphamide plus corticosteroids produces better results than corticosteroids when used alone. However this combination in lupus nephritis patients significantly increases the risk of side effects such as amenorrhea (stoppage of menstrual cycles), cervical dysplasia (abnormalities in cells of the cervix), herpes zoster and infection. A lower dose of cyclophosphamide used along with azathioprine maintenance therapy could possibly reduce this complication.
Thus, cyclophosphamide or mycophenolate mofetil combined with corticosteroids can be used as initial therapy for lupus nephritis.
Other drugs for treating lupus nephritis that are under investigation include rituximab, belimumab and tacrolimus.
In conclusion, existing treatment options are successful in treating lupus nephritis. Cyclophosphamide or MMF plus corticosteroid combination is an option as a first in line treatment for lupus nephritis. After recovery from disease, azathioprine or MMF combined with a corticosteroid is best suited as maintenance treatment.
Reference: Current Therapies for Lupus Nephritis; Zachary et al; US Pharmacist 2012
Source-Medindia
 MEDINDIA
MEDINDIA



 Email
Email