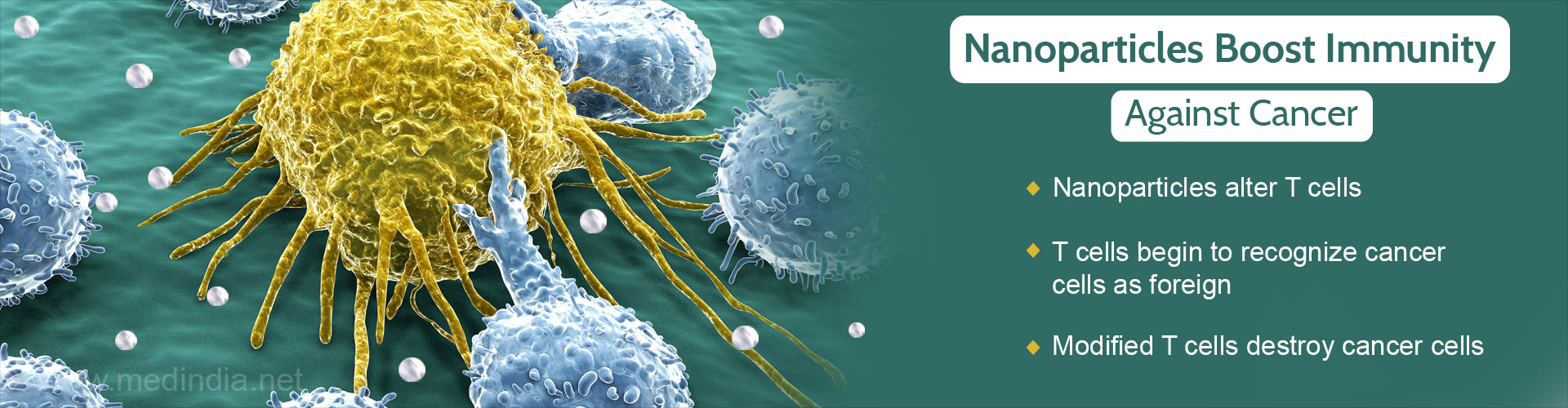
Nanoparticles can be used to modify immune cells to fight against cancer cells, providing a potential therapy for cancer.
- Scientists from Fred Hutchinson Cancer Research Center have developed nanoparticles that modify T cells.
- The modified T cells fight against cancer cells and are a potential method of cancer therapy.
- This method involves modification of the T cells within the body of the patient.
TOP INSIGHT
Cancer cells are the body’s own cells, so T cells do not recognize them as abnormal. Nanoparticles alter T cells to fight against cancer cells.
An alternative to the current treatment methodologies for cancer is necessary, considering the side effects associated with chemotherapy and radiotherapy procedures. Immunotherapy for cancer treatment has been found to show promise in clinical trials that have been conducted but they have been found to have the following limitations:
- It takes many weeks to design immunotherapy interventions
- The T cells, using the currently available procedures, are removed from the patient and then altered, before they are added back into the patient.
- This takes an extended period of time and is both time-consuming and expensive.
Genetic Engineering Within the Body
The nanoparticle engineered T cells would help in providing cellular immunotherapy for cancer patients. The genetic alterations in T cells that occur in a laboratory during traditional immunotherapeutic strategies are now carried out within the body, resulting in an army of T cells against cancer.In the study, Dr. Stephen and his colleagues
- Developed nanoparticles that were bio-degradable
- Altered T cells into CAR (Chimeric Antigen Receptors) T cells
- Designed a promising cellular immunotherapy that has been previously shown to be effective against leukemia
Chimeric Antigen Receptors
The genetically altered T cells are modified to present receptors on their surface which are called chimeric antigen receptors (CARs). These protein receptors are utilized by the T cells to recognize tumor cells. In the traditional method of immunotherapy, these CAR T cells are cultured in the laboratory till they are present in billions. When there are significant CAR T cells, these cells are introduced into the patients. The T cells would then multiply within the body and, with the help of their chimeric receptor, recognize and kill the cancer cells.The difference in the system in the current method of immunotherapy involves
- Nanoparticles contain genes that are necessary for the development of the chimeric antigen receptors.
- The nanoparticles are tagged which helps them in getting attached to T cells.
- The nanoparticles are then engulfed by the T cells
- Once inside the T cells, the nanoparticles are directed towards the nucleus, where they dissolve.
- The new Chimeric Antigen Receptor (CAR) genes from the nanoparticles integrate with the chromosomes that are present in the nucleus.
- The CAR genes provide the necessary information for the T cells to present cancer receptors on its surface, within a period of a day or two.
- One group of mice was treated with traditional chemotherapy procedures.
- One group of mice was treated with the nanoparticles.
The findings of the study revealed that
- The mice which were treated with the nanoparticles modified T cells showed an improvement in survival by 58 days.
- This is a significant increase in survival from the 2 weeks that the control mice survived with leukemia.
References:
- Tyrel T. Smith, Sirkka B. Stephan, Howell F. Moffett, Laura E. McKnight, Weihang Ji, Diana Reiman, Emmy Bonagofski, Martin E. Wohlfahrt, Smitha P. S. Pillai, Matthias T. Stephan. In situ programming of leukaemia-specific T cells using synthetic DNA nanocarriers. Nature Nanotechnology, 2017; DOI: 10.1038/nnano.(2017).5
- CAR T-Cell Therapy: Engineering Patients’ Immune Cells to Treat Their Cancers - (https://www.cancer.gov/about-cancer/treatment/research/car-t-cells)
Source-Medindia
 MEDINDIA
MEDINDIA


 Email
Email