Chronic kidney disease (CKD) can be used as a model for improving chronic disease care using electronic health records (EHRs), says a new study.

The US researchers also outline specific design features for incorporating CKD-related data into EHRs.
The researchers concluded that though these strategies may be most effectively applied in the setting of CKD, they may also apply to other chronic diseases.
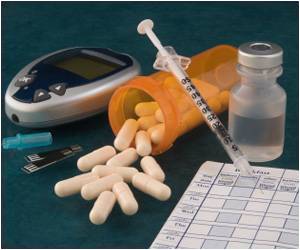
CKD (also known as chronic renal disease) is a medical condition characterized by a gradual loss of renal function over time. According to the National Health Foundation, US, about 10% of the world population is affected by CKD. Generally, objective laboratory data defines CKD and related conditions and clinical care needs combined effort from a diverse team of health care professionals. However, CKD detection and management should see more improvement.
According to the researchers, well-designed EHRs will be helpful for clinicians to care for patients with CKD or other chronic diseases. Such efficient electronic records can also increase the continuity of services, facilitate association between providers, and support patient self-management.
Apart from clinical benefits, EHRs can increase our understanding of diseases as they can provide rich data for observational studies and recognize potential patients for research. EHRs can also give in-depth data to national surveillance systems to enable targeted strategies for upgrading public health.
With this in mind, the US researchers chalked out general strategies for using EHRs to improve care and treatment for patients with CKD. They also developed specific design features and goals for incorporating the chronic disease data into EHRs.
The researchers conclude that several characteristics make CKD an ideal model for recognizing and developing strategies for designing and using EHRs to allow clinicians to treat people better with chronic conditions.
"CKD is common and its care is suboptimal, allowing significant room to show improvement as EHRs are optimized, and because CKD is defined by objective data, the disease is an ideal example of a condition that can be easily identified by information commonly found in EHRs," said Dr. Patel.
Dr. Patel also said CKD care needs long term association between diverse professionals across numerous healthcare frameworks, which could be facilitated by EHRs.
“Furthermore, CKD often heralds increased risk for hospitalizations, cardiovascular events, and all-cause mortality, so EHR-based improvements in CKD management may in turn improve care for these related conditions," said Dr. Patel.
Reference
Clin J Am Soc Nephrol. 2015 Aug 7;10(8):1488-99. doi: 10.2215/CJN.00940115. Epub 2015 Jun 25.
http://www.eurekalert.org/pub_releases/2015-06/ason-tie061915.php
Source-Medindia
 MEDINDIA
MEDINDIA

 Email
Email